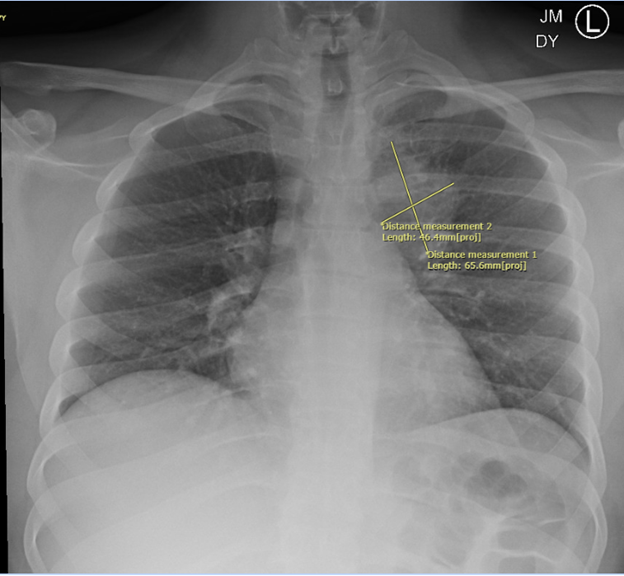
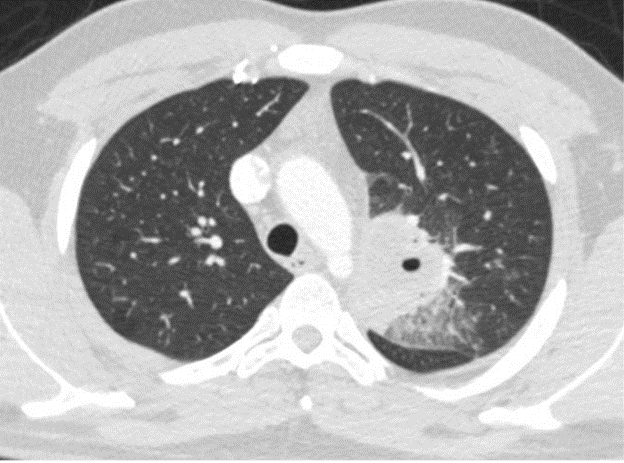
Case Presentation: Case: A 27-year-old male presented to the emergency room with fever, night sweats, and productive cough with brown sputum for the past week prior to presentation. He also noted associated anorexia, nausea, and non-bilious, non-bloody vomiting. The patient reported persistent dysphagia that had developed after his laryngeal schwannoma resection 15 years ago. On presentation, he was febrile to 100.4 degrees Fahrenheit, tachycardic to 102 beats per minute, and tachypneic to 37 breaths per minute. Physical exam was within normal limits. Labs were notable for neutrophil-predominant leukocytosis (WBC: 14.37 × 109/L) and elevated inflammatory markers. Computerized tomography of the chest demonstrated a focal necrotic air-filled lesion in the posterior left upper lobe consistent with lung abscess. The patient was admitted for management of lung abscess with parenteral antibiotics. He was started on ampicillin-sulbactam and demonstrated substantial clinical improvement. Sputum cultures grew normal respiratory flora. Videofluoroscopic swallowing study demonstrated moderately compensated oropharyngeal dysphagia. His course was complicated by drug-induced liver injury secondary to ampicillin-sulbactam and was switched to a four-week course of levofloxacin and metronidazole. He was discharged with close follow-up with his primary care provider, otolaryngology, pulmonology, and speech and language pathology.
Discussion: Background: Lung abscesses commonly occur as a result of aspiration3 and are often seen in individuals with oropharyngeal dysphagia6. Laryngeal schwannomas are rare, benign tumors of the Schwann cells surrounding the larynx. Local growth can cause compressive symptoms of surrounding structures resulting in dysphonia, globus sensation, oropharyngeal dysphagia, stridor, and dyspnea2. The definitive treatment for these patients is surgical resection1, which is curative in most cases5. However, the prevalence of long-standing complications post-resection is not well defined. We present a unique case of a young individual presenting with a lung abscess in the setting of remote laryngeal schwannoma resection. On review of current literature, the most common predisposing factors for lung abscesses include alcoholism, seizure disorder, and history of stroke2. Some studies cite pharyngeal surgery as another potential risk factor; however, most available literature comments on cases of individuals with a prior history of laryngectomy in the setting of malignancy2,7. Vocal cord schwannomas are rare, as a result, long-term complications of surgery are not widely reported. In a small case series, 66% of individuals developed oropharyngeal dysphagia 10 months after schwannoma resection3, indicating that resection may be an underrecognized risk factor for aspiration.
Conclusions: Conclusions: Consultation with speech-language pathologists is essential for preventing further aspiration events, therefore identifying longstanding dysphagia in patients is vital in optimizing care4. This vignette highlights the importance of evaluating aspiration risk in patients with a history of benign vocal cord tumors, as well as the need for multidisciplinary management of lung abscess in these populations.