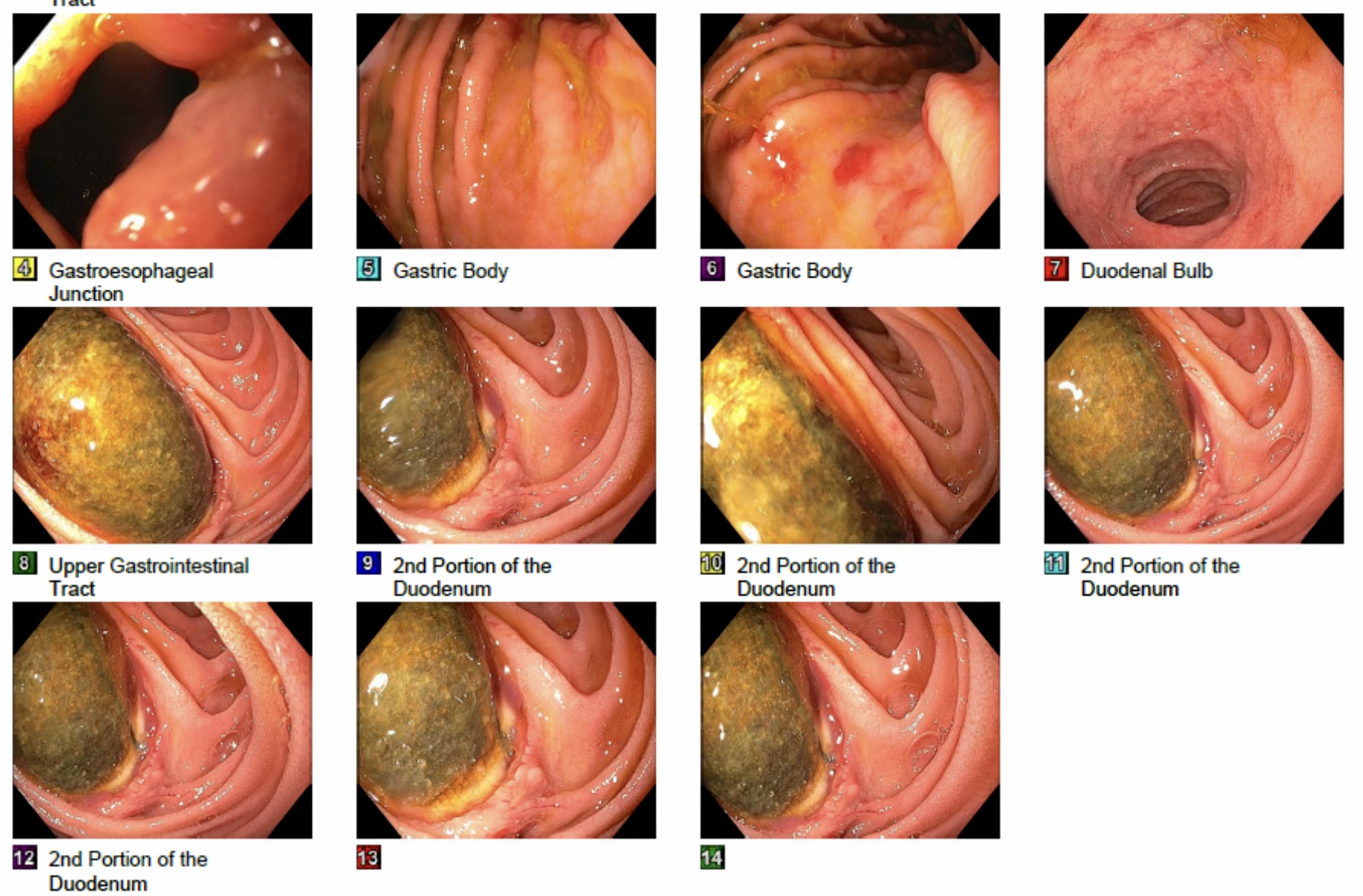
Case Presentation: 56-year-old man with past medical history of abdominal aortic aneurysm surgery was brought to the Emergency Room for change in mental status and having bloody vomitus and melenic stool. On admission, abdominal exam was unremarkable, blood pressure was 110/77 mmHg, heart rate 103/min, Temperature 99.8 °C, Respiratory rate 20 per minute, hemoglobin 11.1 g/dl, WBC 32400 cells/mcl, and platelet 312000/mcl. Patient was intubated on arrival for airway protection. CT Abdomen/Pelvis with IV and oral contrast revealed ectasia of the mid to distal part of abdominal aorta measuring 2.5 x 2.4 cm with no leakage of contrast outside the aorta. Upper GI endoscopy revealed one non-obstructing duodenal ulcer with aortic graft eroding through. Patient was emergently taken to the operating room, exploratory laparotomy showed two areas of small bowel tenaciously adherent to the previous aortic graft, one in the 4th portion of duodenum and one in the distal jejunum. Fistulas were repaired and an aortic stump was placed. Therefore, wide debridement and irrigation were performed. Escherichia coli and Candida were isolated from the graft culture. Antibiotics were modified and supportive care resumed. Patient was extubated 2 days after the surgery and transferred to a skilled nursing facility to complete a total of 6 weeks of IV antibiotics and lifelong antifungals.
Discussion: The incidence rate of secondary AEF is 0.3%-1.6% [3]. One study of PAEF in dogs demonstrated a role for both mechanical factors and aortic inflammation/infection in their development [4]. Aortoduodenal fistulas are the most common AEF [5]. In our patient, marked signs of infection around the fistulas have been suggesting that the fistula arises from prosthesis infection. CT angiography is the first-line imaging modality for evaluating suspected bleeding [6,7], followed by endoscopy and arteriography. Treatment options for AEF are graft excision and establishing an extra-anatomic bypass, in situ graft replacement, and simple graft excision alone. Endovascular repair is an alternative therapeutic option. Broad-spectrum antibiotics should be initiated immediately with coverage for Gram-positive, Gram-negative, and anaerobes. Fungal infections of the vascular graft are rare [8], however, in our patient it came positive for Candida. The presence of Candida and polymicrobial bacteria in blood in a patient presenting with GI bleeding may suggest an aortoduodenal fistula and help in diagnosing this life-threatening condition [9].
Conclusions: Aortoenteric fistula is a life-threatening condition associated with high morbidity and mortality and it can also pose a diagnostic dilemma. There are many mimics of AEFs including perigraft infection without fistulization, retroperitoneal fibrosis, infected aortic aneurysm, and infectious aortitis. AEF should always be on the differential in patients presenting with GI bleeding who have a history of abdominal aortic aneurysm repair. Also, aortoduodenal fistula should be strongly suspected in any patient with a history of aorta repair presenting with GI bleeding and candidemia. Prompt diagnosis and early surgical intervention are required to prevent a lethal outcome.