Background: High flow nasal cannula (HFNC) is a non-invasive oxygen delivery system commonly used in emergency rooms, pediatric intensive care units (PICU), and pediatric wards for respiratory illnesses. Previously, HFNC was strictly managed in the ICU, but this is becoming less common as more pediatric wards have initiated its use. Questions have arisen regarding the safety and utilization of HFNC use in the wards. In addition to previously examined safety factors, we studied hospital cost, rate of transfer to outside facilities, use of medications and length of time on HFNC. Our study includes patients managed for all pediatric respiratory illnesses, not only bronchiolitis as in prior studies. Our institution’s unique perspective examines the early stages of this change in the pediatric ward during the 2022/2023 RSV surge and bed crisis vs. hospitals that have been well established in their usage.
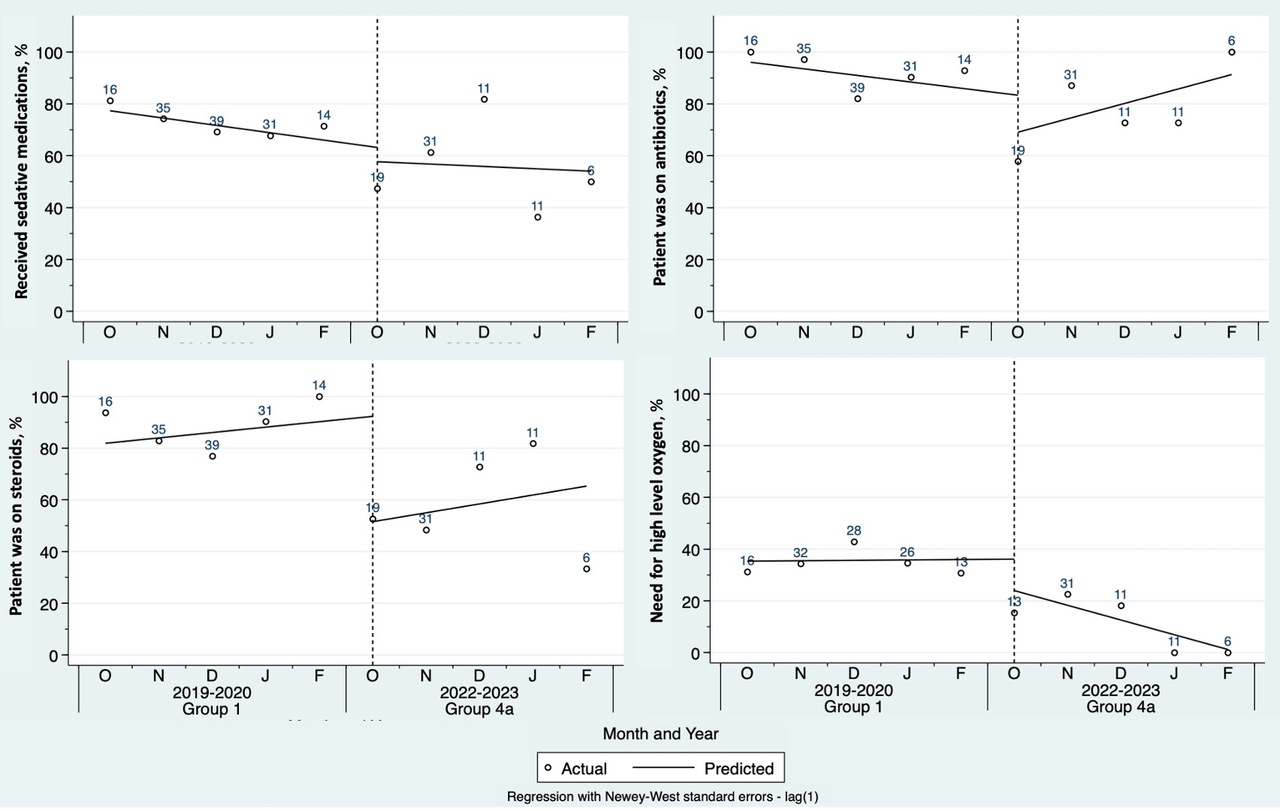
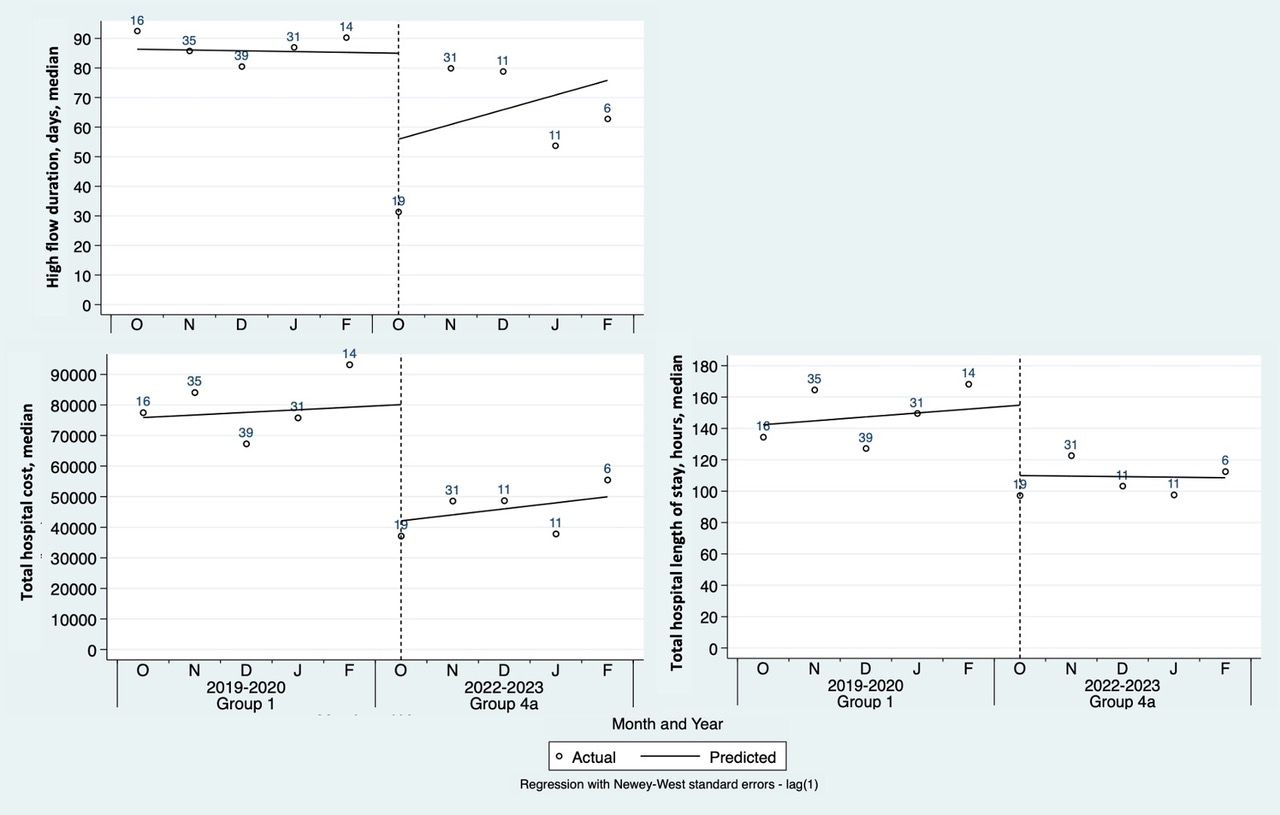
Methods: This retrospective chart review examined patients ≤17 years old managed on HFNC for a primary respiratory illness on the pediatric ward from October 2022 to February 2023 (viral season 2022) and compared them to patients on HFNC in the PICU from viral seasons 2019 to 2022. Patient’s with complex medical history were excluded. We examined rates of ER initiated HFNC patient transfers to outside facilities, and compared variables associated with respiratory illness, medical management, length of stay (LOS), and hospital costs for all viral seasons. Binary and categorial variables were compared by Chi-squared or Fisher’s exact tests. Continuous variables were analyzed using univariable linear or quantile regression. Trends were assessed using a weighted interrupted time-series analysis.
Results: HFNC patients on the pediatric ward compared to the PICU had shorter LOS and duration of time on HFNC. There was no increased need for higher-level ventilation therapy for HFNC patients started on the ward. This overall led to decreased hospital cost. HFNC patients initiated on the ward had lower use of steroids, antibiotics, and sedative medications (Table 1). No differences were observed for use of albuterol or narrow vs broad spectrum antibiotics. While there was an observed decrease in institutional transfers after initiation of HFNC use in the ward setting, it was not statistically significant.
Conclusions: Decreased hospital LOS, hospital cost, and utilization of medications were observed for patients initiated on HFNC on the pediatric ward vs the PICU, without an increased risk of higher-level ventilation use during pediatric bed crisis in a hospital with newly established HFNC protocols.