Background: Cannabinoid Hyperemesis Syndrome (CHS) is a rare condition first reported in adolescent patients in 2010. It is associated with episodic abdominal pain, emesis, and intractable nausea which resemble cyclical vomiting syndrome (CVS) in the setting of chronic use of cannabis. (5,12). Evidence of CHS treatment effectiveness in children is limited to case studies and extrapolated adult evidence. Treatment failures have been reported with various antiemetic drugs, including ondansetron, promethazine, metoclopramide, and diphenhydramine, despite different formulations, routes, and dosages (9). Benzodiazepines such as Lorazepam and Clonazepam have been reported as effective pharmacologic therapy for adolescents experiencing acute CHS symptoms (7). Previous case series have suggested that capsaicin cream, benzodiazepines, and Haloperidol are more effective at reducing acute symptoms compared to customary anti-emetic therapies like Ondansetron (2,3,7). There is a lack of knowledge regarding the length of time required for symptom resolution after cessation of cannabis products. However, sustained cessation has been universally demonstrated as the only intervention with longitudinal efficacy (5,6,9).
Methods: A single institution retrospective record review from 2016 to 2022 of patients aged 11-21 years who presented to a 309-bed tertiary care children’s hospital. Inclusion considerations were based on CVS adult ROME IV criteria of stereotypical episodic vomiting with presentation after excessive cannabis use. Effectiveness was defined as cessation of symptoms (nausea, emesis, abdominal pain) 24 hours after administration of medication and was collected from a single patient encounter for each patient. 204 encounters were included, and 46 unique patients were identified.
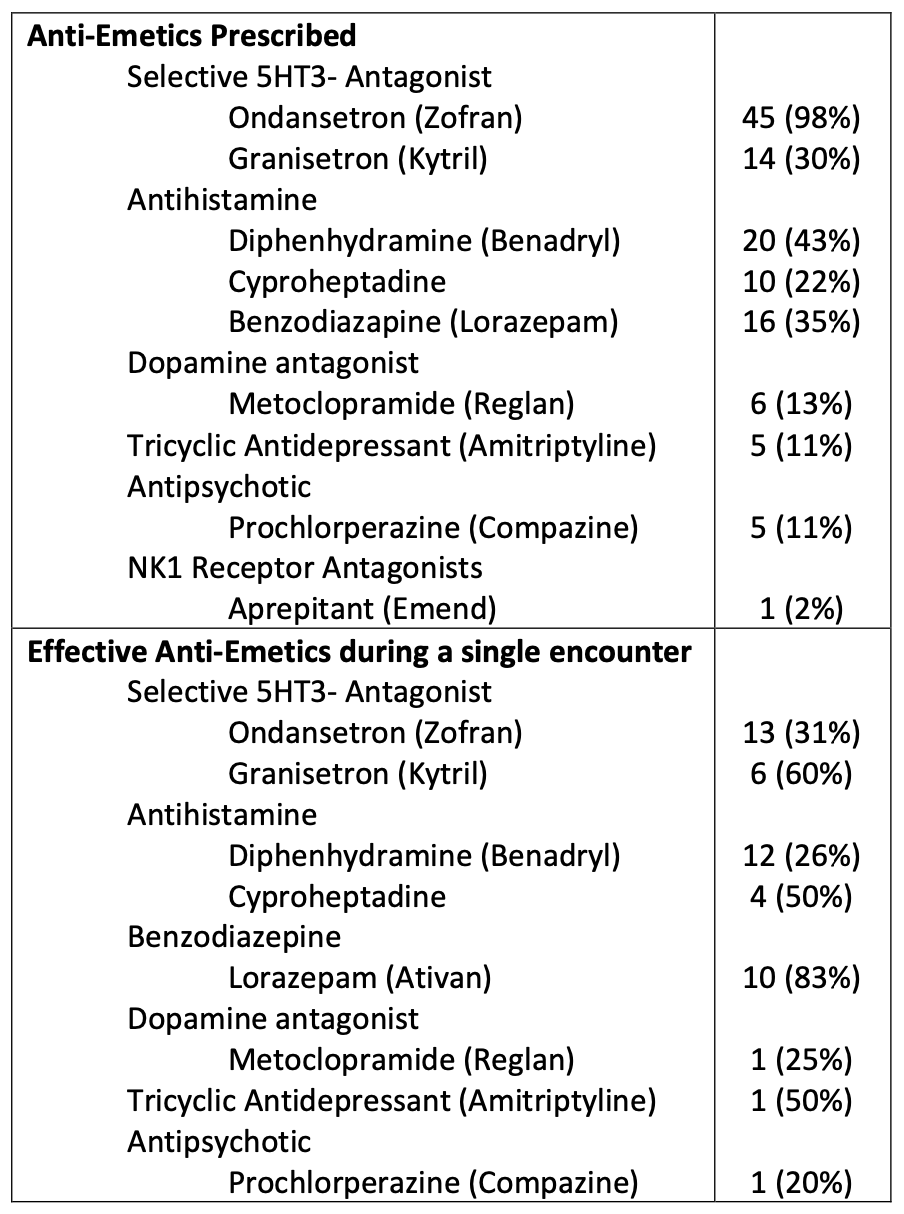
Results: 46 patients (23 females and 23 males) with a mean age of 17 accounted for 204 emergency department and inpatient encounters. A wide variety of anti-emetics including selective 5-HT3 antagonists, antihistamines, benzodiazepines, and tricyclic antidepressants were prescribed. Among the patients, 41% did not respond to any medication. Ondansetron was administered in 98% of the patient encounters and was found to be effective in 31% of the cases, mostly when used in combination with other medications. Lorazepam had an effectiveness rate of 83%. Diphenhydramine was the second most commonly administered medication, given to 43% of the patients, its effectiveness rate was 26%. Granisetron was effective in 6 out of 10 patients (60%), while Cyproheptadine was effective in 4 out of 9 patients (44%).
Conclusions: Traditional antiemetic therapies are often prescribed, but studies continue to show that they are not effective. Ondansetron was the most used anti-emetic but was only effective in 31% of cases. On the other hand, Lorazepam was prescribed to one-third of the patients and was found to be 83% effective in improving symptoms, making it the most successful medication measured in this study followed by Granisetron and Cyproheptadine. In many cases, multiple antiemetics were prescribed, making it unclear which one was the most beneficial. Efforts should be made to establish pediatric-specific diagnostic criteria as well as to validate abortive and prophylactic treatment algorithms.