Background:
There is an increased focus on measuring and improving quality of care for hospitalized older patients. Ideally, adherence to quality measures is associated with improved outcomes for these patients. This study aimed to assess the relationship between quality of care, measured by ACOVE (Assessing Care of Vulnerable Elders) quality indicators (Qls), and survival 1 year after discharge for frail older inpatients.
Methods:
Inpatients age 65 and older admitted to an inpatient general medicine service at a single academic medical center were invited to participate in an admission interview. Patients who died in the hospital, were discharged to hospice, or transferred from an ICU were excluded. Those patients identified as vulnerable using the Vulnerable Elders Survey (VES‐13) received a full assessment of ADLs and a medical chart review for adherence to 16 ACOVE Qls. A composite quality score reflecting perent adherence to 16 ACOVE Qls was calculated. Postdischarge death date was obtained from the Social Security Death Index. Multivariate logistic regression and Cox proportional hazards models, controlling for demographics and other possible confounders (VES‐13 score, baseline ADL limitations, DNR/DNI status, length of stay, Charlson index, and number of Qls triggered) were used to assess the relationship between quality of care (quality score and adherence to individual Qls) and postdischarge mortality.
Results:
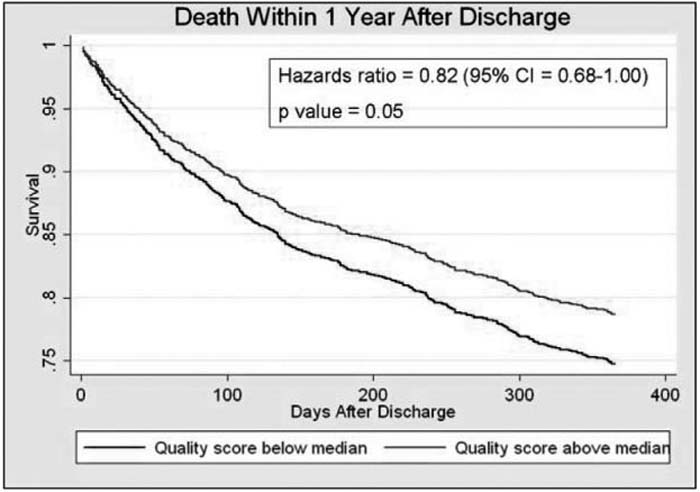
From May 2004 through June 2007, 3356 older patients (69%) agreed to participate. Of these, 1861 (56%) were identified as vulnerable. To date, 1856 chart reviews (99%) have been completed. Patients triggered a mean of 8.3 Qls (SD 2.0 Qls). Mean quality score was 59.3% (SD 19.2%). Four hundred and ninety‐five patients (27%) died within 1 year of discharge. Multivariate logistic regression demonstrated that a 10% increase in quality score was associated with a 7% decrease in the odds of death 1 year post‐discharge [OR 0.93 (95% Cl 0.87–1.00), P = 0.045]. Using Cox proportional hazards regression, patients receiving a higher‐than‐median quality score were 18% less likely to die 1 year after discharge [HR 0.82 (95% Cl 0.68–1.00), P = 0.05]. This relationship was particularly significant for assessment of nutritional status, which was associated with a 39% reduction in mortality 1 year after discharge [HR 0.61 (95% Cl 0.40–0.93), P = 0.022].
Conclusions:
Higher quality of care for hospitalized vulnerable elders, as measured by ACOVE quality indicators, was associated with improved survival 1 year after discharge. This relationship was particularly significant for older patients receiving inpatient nutritional assessments. Possible mechanisms for these findings include: (1) better quality of care improves posdischarge survival, (2) inpa‐tients who will live longer receive higher quality of care, or (3) adherence to certain process of care measures is a proxy for an unmeasured variable influencing survival. Future research should aim to confirm possible mechanisms for these findings.
Author Disclosure:
M. Fish, none; V. M. Arora, Hartford Foundation, NIA, AHRQ, NIGMS, ACS, ABIM, research funding, Consultant; A. Basu, NIMH, research funding; Jared Olson, none; C, Plein, none; K. Suresh, ACS, Research Funding; G. Sachs, Al‐zheimer's Association, NPCRC, AHRQ, NCRR, NIA, CVS Care, grants, consultancies; D. O. Meltzer, AHRQ, NIA, NIGMS, Pfizer, Merck, RWJ, PeopleChart, research funding, Consultant.