Background: Venous thromboembolism (VTE) is a prevalent and costly medical condition in hospitalized patients. Risk assessment tools like the Padua Predictive Score aim to differentiate low-risk and high-risk patients for targeted pharmaceutical prophylaxis (pPPX) administration. However, widespread adoption of risk assessment remains suboptimal. This study investigates HA VTE prophylaxis use in medicine inpatients within a large integrated health system and compares prophylaxis orders at admission between two different risk stratification methods: a retrospective EHR-based Padua score (ePaduaKP) and the admitting clinicians’ assessment of HA VTE risk based on orderset choice of low, moderate and high risk classification.
Methods: We analyzed data for adult patient hospitalizations at Kaiser Permanente Northern California hospitals from January 1st 2013 to December 31st 2019, excluding intensive care unit (ICU) patients, surgical inpatients, and those already on anticoagulants. We calculated an Electronic Padua Predictive Score (ePaduaKP) for all hospitalizations in this cohort using a previously described method and electronic health record (EHR) data (Neeman et al 2022). For a smaller subset of hospitalizations (from January 1st 2018 to December 31st 2019), we also extracted the admitting clinicians’ documented assessment of HA VTE risk through EHR orderset selections.
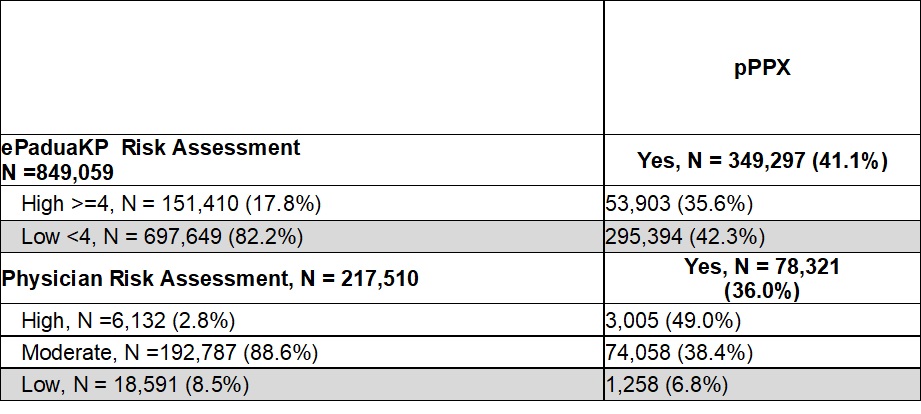
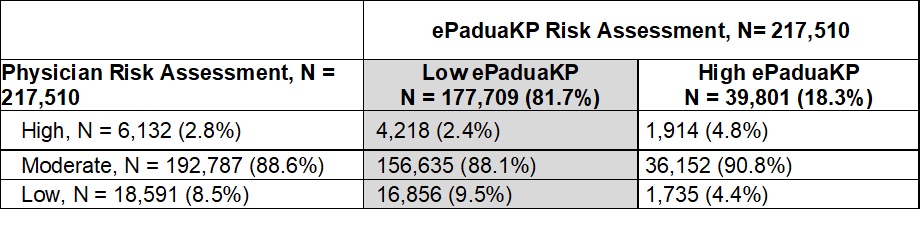
Results: Out of 849,059 encounters, 82.2% were classified as low risk by ePaduaKP, among which 42.3% received pPPX. Overall, 41.1% of these encounters received pPPX. In the subset of 217,510 encounters where clinician assessment data was available, 81.7% were deemed low risk by ePaduaKP. In contrast, 88.1% and 9.5% were assessed as moderate and low risk, respectively, by admitting clinicians. Within this smaller cohort, 36% of encounters received pPPX. Specifically, 38.4% and 6.8% of those assessed as moderate and low risk by admitting clinicians, respectively, received pPPX.
Conclusions: A discrepancy existed between pPPX use and HA VTE risk assessment. While most encounters were classified as low risk by ePaduaKP, a considerable number still received pPPX. Additionally, a discrepancy was observed between ePaduaKP risk classification and the admitting clinicians’ assessment of HA VTE risk, with most encounters being classified as moderate risk by admitting clinicians. We hypothesize that admission orderset design choices, including the use of priming words and a ternary risk stratification for a binary clinical decision, may have influenced the high prevalence of admitting clinicians classifying encounters as moderate risk, potentially impacting subsequent pPPX use.