Background: Nationwide, hospitals are experiencing high patient volumes, attributed to medical complexity, hospital length of stay, and hospital readmissions, among other factors. In this context, hospitalists’ roles have been expanding to optimize care during and following hospitalization. Post-discharge care is typically managed by primary care providers, and there is sparse information on programs that leverage hospitalists and digital platforms to improve post-discharge care.
Purpose: The purpose of Post-discharge Early Assessment via Remote video Link (PEARL)–Homeward was to improve the hospital-to-community transition of care with use of a digital platform. The goals of PEARL–Homeward were to (i) facilitate safe, early hospital discharge from hospital medicine services (ii) provide seamless post-discharge follow-up through a digital platform, and (iii) provide remote patient monitoring (RPM). PEARL–Homeward provides time-bound follow-up and transitions care to the primary care provider.
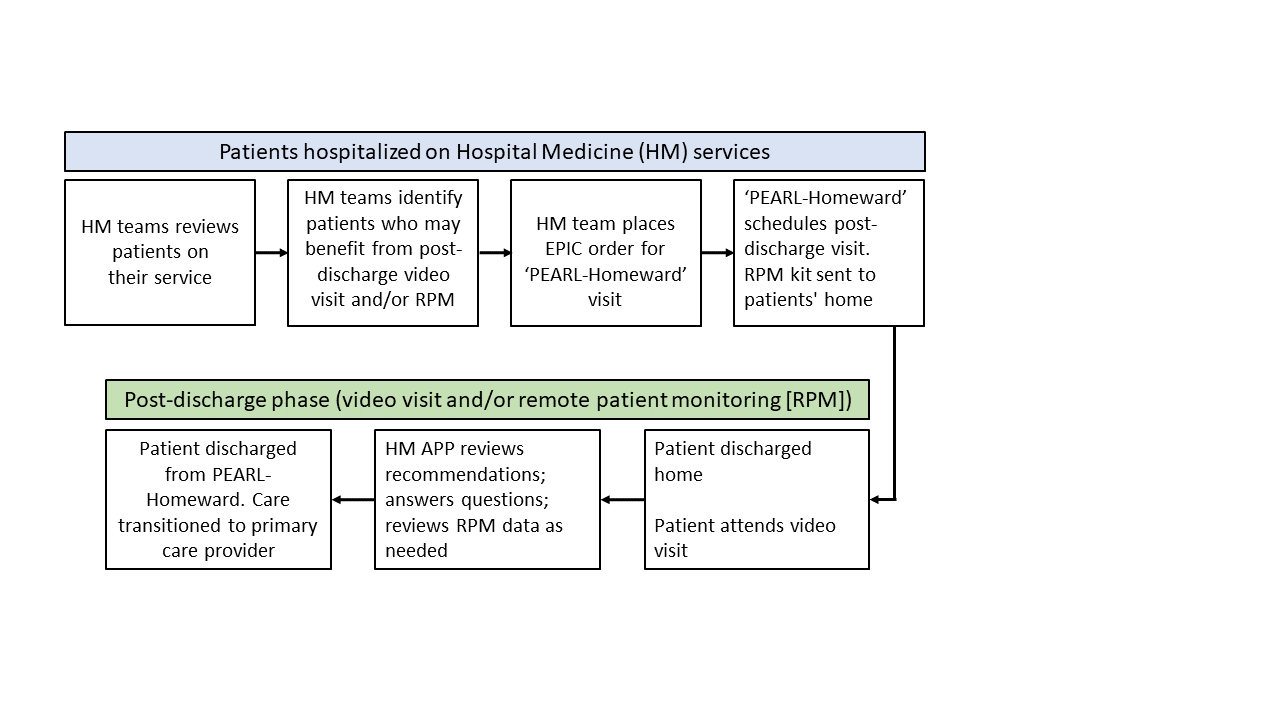
Description: In April 2020, in response to the COVID-19 pandemic, the Division of Hospital Internal Medicine (HM) at a tertiary care center developed PEARL to provide video visits and improve patient adherence to hospital discharge recommendations. In August 2022, PEARL was transformed, and a new phase was formed (goals, above). PEARL–Homeward was formed with 12 multidisciplinary groups/services (eg, Practice Optimization and Acceleration, Center for Digital Health, Hospital Operations) to transform care transitions. From August 2022–March 2023, PEARL–Homeward developed EPIC workflows, integrated appointments and video links into the patient portal, developed educational materials, and then launched. In June 2023, PEARL−Homeward integrated RPM for COPD, hypertension, heart failure, and respiratory illnesses including COVID-19. RPM allows for interval monitoring of vital signs with nursing support. At present, hospitalists (physicians and advanced practice providers [APPs; nuse practitioner or physician assistant]) identify patients on their service who may benefit from a post-discharge video visit and/or RPM and place an EPIC order for PEARL–Homeward. This facilitates early hospital discharges. PEARL–Homeward follow-up is scheduled, patients receive education on Zoom® technology, and if eligible, receive an RPM kit at home. PEARL–Homeward visits are conducted by an HM APP. A desk operations specialist manages the calendar and checks patients in for the video visit. During the video visit, the APP reinforces discharge recommendations, answers questions, and closes care gaps (e.g., provide prescriptions). PEARL–Homeward operates on weekdays from 7:00 am to 5:00 pm.Since March 2023, 32 APPs provided post-discharge video visits to ~300 patients, with ~20 receiving RPM. The patient no-show rate for video visits was 15% (vs. 35% pre-launch). Based on preliminary analysis, the 30-day readmission rate was 21.3% (vs. 24.9% pre-launch).
Conclusions: PEARL–Homeward was developed to improve transitions of care for hospital medicine patients. Workflows were integrated into EPIC to provide seamless video visits and RPM. PEARL–Homeward is being considered by other divisions to improve care transitions. PEARL–Homeward is a departure from the status quo of hospital medicine’s primary responsibilities but reflects the growing importance of hospital medicine across the care continuum. PEARL–Homeward may be adapted at other institutions planning similar initiatives.