Background:
The role of a hospitalist in treating nicotine withdrawal using counseling and medications during hospitalization can improve cessation rates of tobacco users. Clinical decision support and drug-condition alerts within the electronic medical record prompt the prescribing of medications for tobacco treatment and ease documentation of reimbursable counseling by physicians. Additionally, several hospitals have implemented a tobacco treatment service (TTS) to counsel tobacco users and recommend medications for nicotine withdrawal management and for cessation during the hospital admission. While the TTS increases the delivery of treatment, patient abstinence from tobacco significantly increases when a physician provides treatment. The objective of this study was to determine the rate of nicotine replacement therapy (NRT) prescribing during hospitalization and at discharge, as well as the frequency of physician counseling.
Methods:
We conducted a retrospective cohort study of 1154 everyday cigarette smokers admitted to the hospitalist service in an academic medical center from March 2015 to August 2015. Outcome measures were rates of NRT orders during hospitalization and at discharge as well as actual NRT use by patients extracted from the electronic health record. Evidence of physician counseling was determined by analysis of billing data. Bonferroni corrected post-hoc comparisons were performed to assess differences by counselor type (physician, TTS, both, or none).
Results:
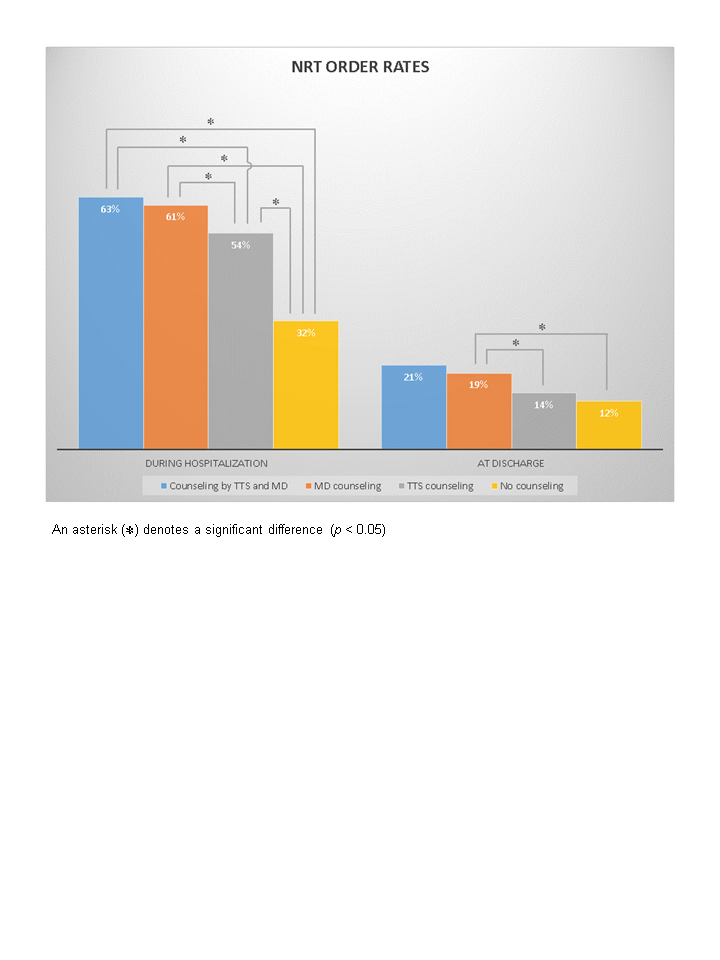
The mean age of patients was 48.5 years and 63% were white. A total of 56% of patients had no documented counseling, 29% of patients were counseled solely by the TTS, 9% had only physician counseling, and 6% had counseling from both TTS and the physician. Physicians counseled a greater proportion of women and African Americans patients. NRT order rates during the hospitalization were highest for patients counseled by both the TTS and the physician (63%) and by physician only (61%), compared to TTS only (54%), and no documented counseling (32%). Orders for NRT at discharge were significantly higher for all counseled patients (TTS and physician counseled [21%], physician only [19%], TTS only [14%]), compared to no documented counseling (12%), and for physician only compared to TTS only. Use of NRT in the hospital was highest for patients counseled by both TTS and physician and lowest for no counseling, and no difference between patients counseled only by the physician compared to TTS.
Conclusions:
Tobacco users who receive physician counseling during their hospitalization have higher rates of nicotine replacement therapy during their hospitalization and added to their list of discharge medications. Although a tobacco treatment service is an important part of providing support to hospitalized smokers, the hospitalist has an essential role in improving tobacco cessation of patients during their hospitalization and post discharge by ensuring they receive effective pharmacotherapy.