Background: An estimated 580,000 individuals were experiencing homelessness during the most recent national point-in-time count. Dialysis requires substantial patient engagement, and not having secure housing impedes medical care and could increase acute care utilization. The prevalence of homelessness and its impact on hospitalizations among patients with ESKD are unknown. This retrospective cohort study examined differences in patient and hospitalization characteristics among adults (aged 18 and above) with ESKD by homeless status using recently added social determinants of health ICD-10 codes.
Methods: Data were collected from the National Inpatient Sample (2016-2020), consisting of all-payer administrative data approximating a 20% stratified sample of all discharges from U.S. community hospitals. Patients with ESKD experiencing homelessness were identified using ICD-10 Z59.0. We compared patient demographic variables and hospitalization characteristics (length of stay, charges incurred, in-hospital mortality) among patients with ESKD by homeless status using chi-squared tests and unadjusted linear regression.
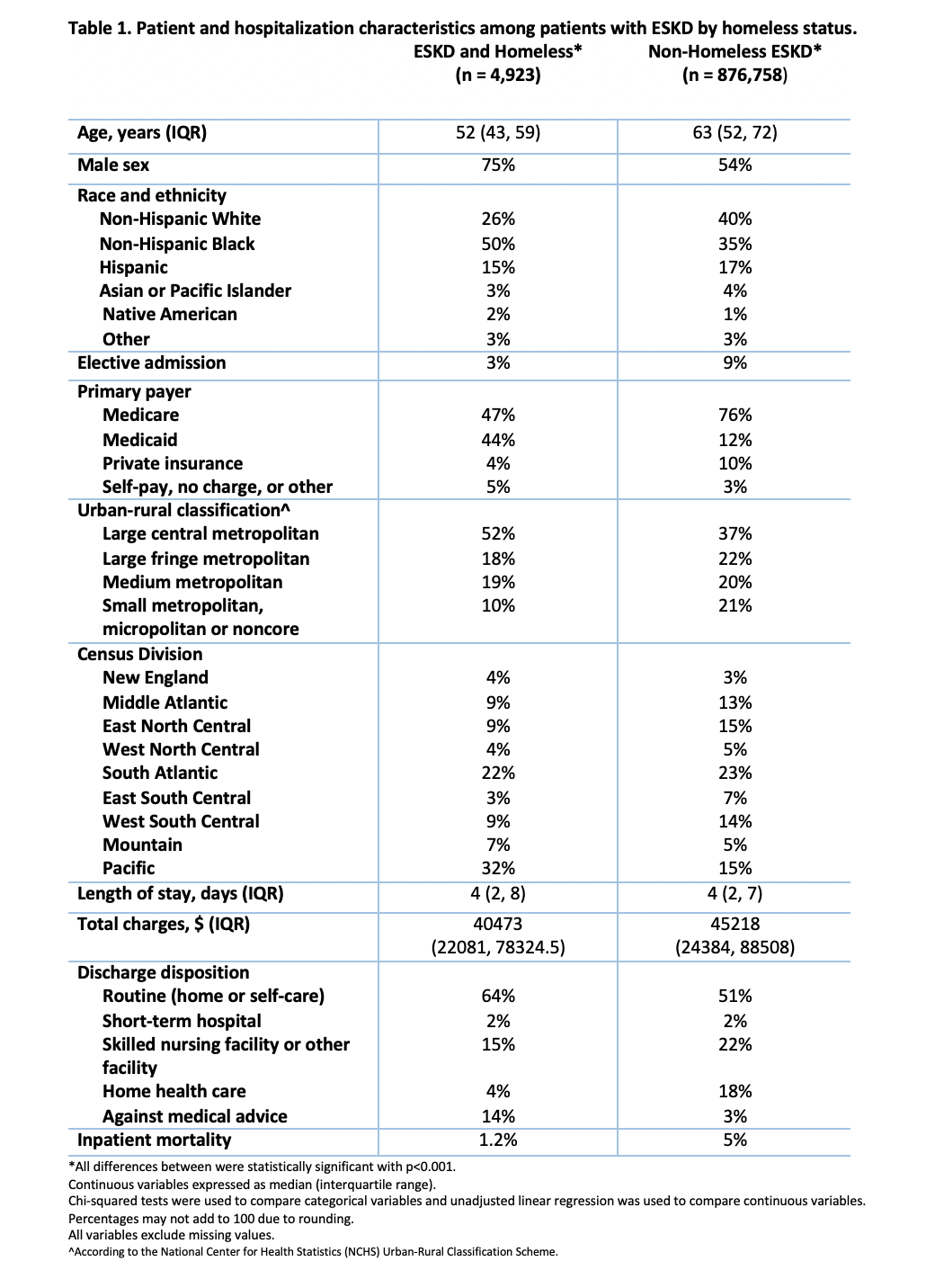
Results: Among 881,681 unweighted hospitalizations for patients with ESKD, 4,923 (0.56 weighted %) had an ICD-10 code for homelessness. Compared with non-homeless patients with ESKD, patients experiencing homelessnesss were significantly younger (median age 52 vs. 63 years, p< 0.001) and more likely to be male (75% vs. 54%, p< 0.001), non-Hispanic Black (50% vs. 35%), have Medicaid as their primary payer (44% vs. 12%, p< 0.001), and reside in large central metropolitan areas (52% vs 37%, p< 0.001).Patients with ESKD experiencing homelessness had a lower likelihood of elective admission (3% vs. 9%, p< 0.001) and incurred lower total charges (median $40,473 vs. $45,218, p< 0.001) during similar hospital lengths of stay (median 4 vs. 4 days, p< 0.001) when compared with non-homeless patients with ESKD. A larger percentage of patients experiencing homelessness were discharged routinely to self-care (64% vs. 51%, p< 0.001) or left against medical advice (14% vs. 3%, p< 0.001) and a lower percentage were discharged to a skilled nursing facility or other facility (15% vs. 22%, p< 0.001). The inpatient mortality rate for patients experiencing homelessness was 1.2%, which was significantly lower than that of non-homeless patients with ESKD (5%).
Conclusions: This study is the first to ascertain differences in patient and hospital characteristics in a national sample of hospitalized patients with ESKD by homeless status. We found that hospitalized adults with ESKD experiencing homelessness were more likely to be younger, of Black race, and covered by Medicaid insurance. We also identified that hospitalized adults with ESKD experiencing homelessness were more likely to be discharged against medical advice and less likely to be discharged to a skilled nursing facility, indicating that homelessness might be a driver of kidney disease disparities. Further research is needed to assess whether these differences in discharge disposition lead to adverse health outcomes and hospital readmission. These findings can inform the development of patient-centered interventions for individuals with ESKD experiencing homelessness to enhance access to care and improve hospitalization-related outcomes.