Background: Optimal patient care requires excellent patient communication skills. These skills are associated with improved patient satisfaction and adherence and may positively impact overall patient care and reduction in readmissions. Standardized patients (SPs) are commonly used in Undergraduate and Graduate Medical Education; however, their use for faculty education is uncommon, despite being considered an effective modality for teaching physicians communication skills. On-boarding of new hospitalist hires to efficiently and effectively acculturate them to their new place of employment is important both for their own career goals and satisfaction, and to ensure consistency in patient care in the new institution. Therefore, all new physician hospitalists attended workshops on improving communication skills at our Academic Medical Center.
Purpose: The goals were:• Teach communication tools for giving bad news and responding empathically to patient’s and family’s emotions
• Give structured feedback on communication skills using Standardized Patients
• Ensure consistency in communication skills
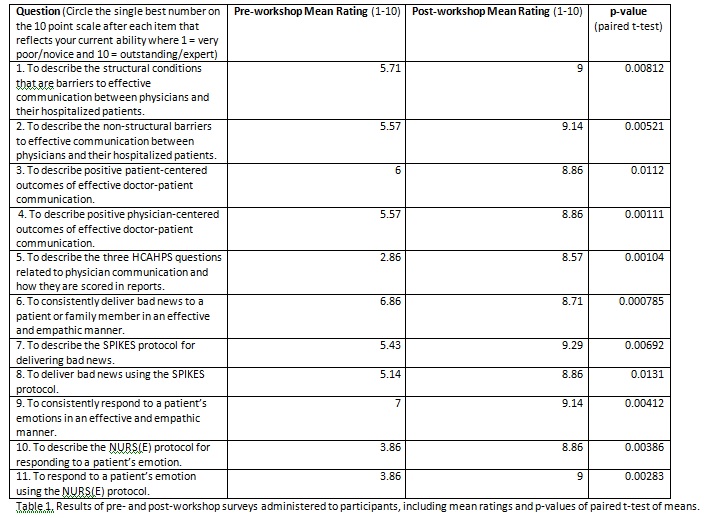
Description: The workshops were given in the Summer of 2017. This workshop was previously given to all our hospitalists between March 2016 and March 2017 as part of a study approved by the IRB as QI. The workshop was designed for 2 or 3 participants as a single 3-to-4-hour session that provided background information on HCAHPS, positive outcomes of effective communication on patients and physicians, and evidence-based general communication skills and specific communication tools for delivering bad news (SPIKES protocol) and responding empathically (NURS[E] protocol). Each learner practiced these skills and tools using a simulated clinical scenario portrayed by SPs. Each learner was provided with immediate feedback about how they communicated with the SPs by peers, faculty facilitator(s) and the SPs. Seven new hires completed the workshop. Pre- and post-workshop surveys of new hires demonstrated statistically significant improvement in all items (see table 1). Items that demonstrated the greatest improvement were knowledge about HCAHPS and self-assessed ability to apply both the NURS[E] and SPIKES protocols. Comments were uniformly positive with the most common one being the desire for greater use of SPs in faculty development.
Conclusions: A communication skills workshop using SPs that aimed to improve physician-patient communication for new hires as part of the on-boarding process at an Academic Medical Center Section of Hospital Medicine was not only well received but also effective based on pre-/post-self-assessments. In addition, SPs may be an underutilized but valuable resource for faculty development.