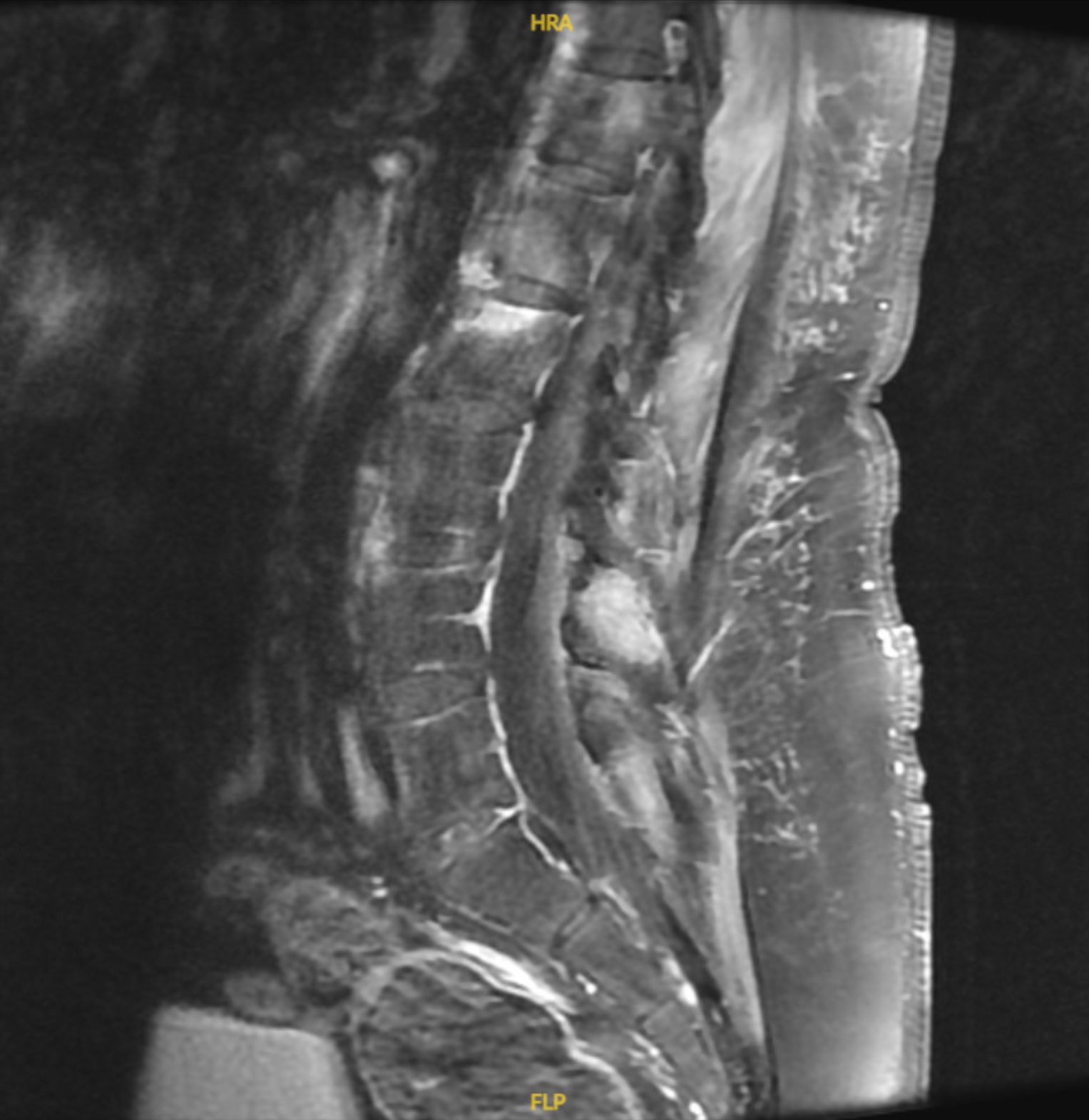
Case Presentation: A 29-year-old African American male with chronic intermittent low back pain of several weeks presented with sudden-onset severe low back pain and inability to bear weight or ambulate. Prior to his hospitalization, he had a few urgent care visits, where he was diagnosed with back pain of muscular origin and was discharged home with over-the-counter pain medications and without spinal imaging. The morning of his hospital admission, he experienced sudden-onset severe low back pain resulting in an inability to stand or walk, requiring hospitalization. Examination did not reveal any focal neurologic deficits. An MRI of the thoracic and lumbar spine demonstrated endplate marrow edema and multifocal areas of enhancement within the thoracic and lumbar spine involving multiple vertebral bodies, intervertebral discs, epidural space and paraspinal soft tissue. Large annular tears of the lateral aspects of L5-S1 were also noted without spinal cord compression. A lumbosacral X-ray showed diffuse sclerosis of the bilateral sacroiliac joints consistent with sacroiliitis and subsequent testing for the HLA-B27 antigen returned positive. The patient was initiated on Ibuprofen and was discharged with outpatient referrals for rheumatology, pain management and physical therapy. He did not demonstrate improvement with initial therapy, but initiation of Adalimumab has demonstrated remarkable improvement in pain and ability to ambulate without a walker.
Discussion: Ankylosing Spondylitis commonly presents as chronic low back pain but severe complications such as pseudoarthrosis and paraplegia have been described. Although, most sudden-onset complications occur in association with trauma, our patient developed sudden-onset symptoms in the absence of trauma. Early identification and management can be critical for patients at risk of such debilitating complications. Initial treatment consists of exercise, physical therapy and NSAIDs with escalation to DMARDs and biologics such as TNF and IL-17 inhibitors, with inadequate response to initial therapy. A disease more commonly reported among Caucasian and Asian populations, it has not been very well described in Blacks. A 2012 study showed a 1.1% prevalence of HLA-B27 in Non-hispanic blacks. Traditionally believed to be more prevalent in young male populations, recent studies have shown that gender, as well, may not predict the incidence of Ankylosing Spondylitis. The patient described in this case was initially misdiagnosed with back pain of muscular origin and did not receive timely identification and management of his Spondyloarthritis and an initial complicated outcome was not prevented.
Conclusions: With the evident health-care disparities in minority groups, this case emphasizes the need for further investigation and re-evaluation of the incidence and prevalence of axial spondyloarthritides in all populations. It also highlights the importance of keeping a broad differential diagnosis and maintaining a lower threshold for performing imaging studies, for common symptoms such as back pain in populations not perceived to be at-risk, particularly in young adults.