Background: Prior exposure to antibiotics is associated with a subsequent risk for sepsis (Baggs et al., 2018). However, there are limited data on characteristics of patients readmitted with sepsis following previous antibiotic exposure during a non-sepsis related hospitalization. We sought to characterize factors associated with sepsis-related readmission (SRR) within 30 days of a non-sepsis index hospitalization that included antibiotic exposure. We hypothesized that patients with SRR have unique characteristics during the index hospitalization.
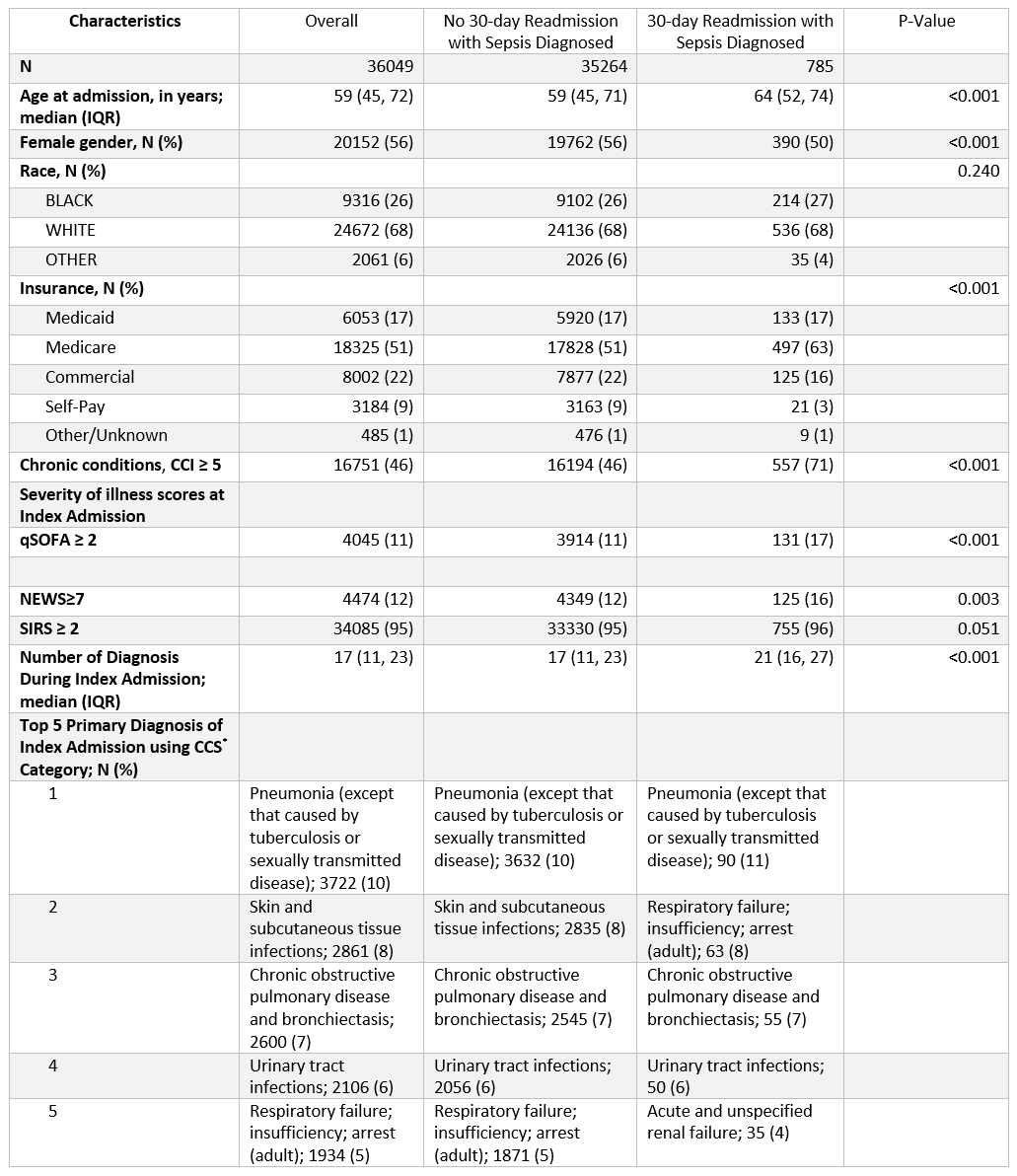
Methods: We identified patients admitted via the Emergency Department with suspected infection (based on culture collection and antibiotic order within 24 hours) and discharged alive without a sepsis diagnosis from 12 affiliated acute care hospitals of the healthcare system in the Southeast of the U.S. between January 2014 and September 2017. Quick-Sequential Organ Failure Assessment (qSOFA), systemic inflammatory response syndrome (SIRS), and National Early Warning Score (NEWS) were calculated during the first 24 hours of the index hospitalization. We also measured Charlson Comorbidity Index (CCI), sociodemographic factors, median number of diagnoses, and the five most frequent primary discharge diagnoses (Clinical Classifications Software) for index hospitalization. The primary outcome was SRR within 30 days of index hospital discharge. We defined SRR as ICD-9 and 10 discharge diagnosis for sepsis, severe sepsis, septic shock, or simple infection plus organ dysfunction (i.e., Angus implementation [Angus et al., 2001]). Multivariable logistic regression modeling was used to evaluate the association between 30-day SRR and patient factors.
Results: We observed 52,184 patients with an index hospitalization for suspected infection, including 2030 who died while hospitalized and 36,049 who were discharged alive without a sepsis diagnosis. Among survivors discharged from the index hospitalization without sepsis, SRR occurred in 785 (2%). Patients with SRR were older (age 64 vs 59; OR=0.99, 95%CI=0.99-1), and more often had CCI ≥ 5 (71% vs 46%; OR=2.2, 95%CI=1.8-2.6) and qSOFA ≥ 2 (17% vs 11%; OR=1.3, 95%CI=1-1.6) on index hospitalization, compared to patients without SRR.
Conclusions: Patients with 30-day SRR following non-sepsis index hospitalization that included early antibiotic exposure have characteristics unique from those without SRR. Chronic conditions and acute severity observable during the index hospitalization may help identify patients at risk for later development of sepsis requiring readmission and facilitate targeted prevention efforts.