Background: Fall for hospitalized patients can cause significant injury and have devastating long term consequences for patients with 33% resulting in injury, 4-6% causing serious injury (1). Information is available regarding risk factors for falls and specific patient or nursing centric interventions to prevent falls, but there is little known about the physician perspective in falls and their direct role in post-fall assessments and secondary fall prevention. The perspective of a physician trainee is even less well known, but potentially even more important as they provide care for a large proportion of patients at most hospitals and especially during off-house. The aim of this study is to evaluate Internal Medicine residents baseline knowledge of fall risk factors, appropriate assessment practices, and opportunities for secondary fall prevention.
Methods: The project was conducted within an Internal Medicine residency program based in an urban, community hospital. Falls were identified as a safety priority at the hospital level, where ongoing fall tracking was being carefully completed, as well as concurrent nursing education on best practices for falls. To perform a current state assessment internal medicine residents were asked to complete a survey to evaluate their understanding of fall risk factors, post-fall evaluation, and fall prevention practices. The survey was designed as free responses with an a priori design for aggregation of terms into specific categories within each question, and it was delivered during noon lecture at the end of academic year (AY) 2019 for all residents and in orientation for new interns of AY2020. A didactic lecture focused on best practices and internal protocols for fall prevention and post-falls assessment, with a focus on medication review, was delivered after completion of the survey. A follow-up survey was completed for all available residents at a subsequent noon conference. Pre-intervention surveys responses were compared between PGY-1s and PGY2-3s and cumulative pre- and post-intervention surveys were also compared.
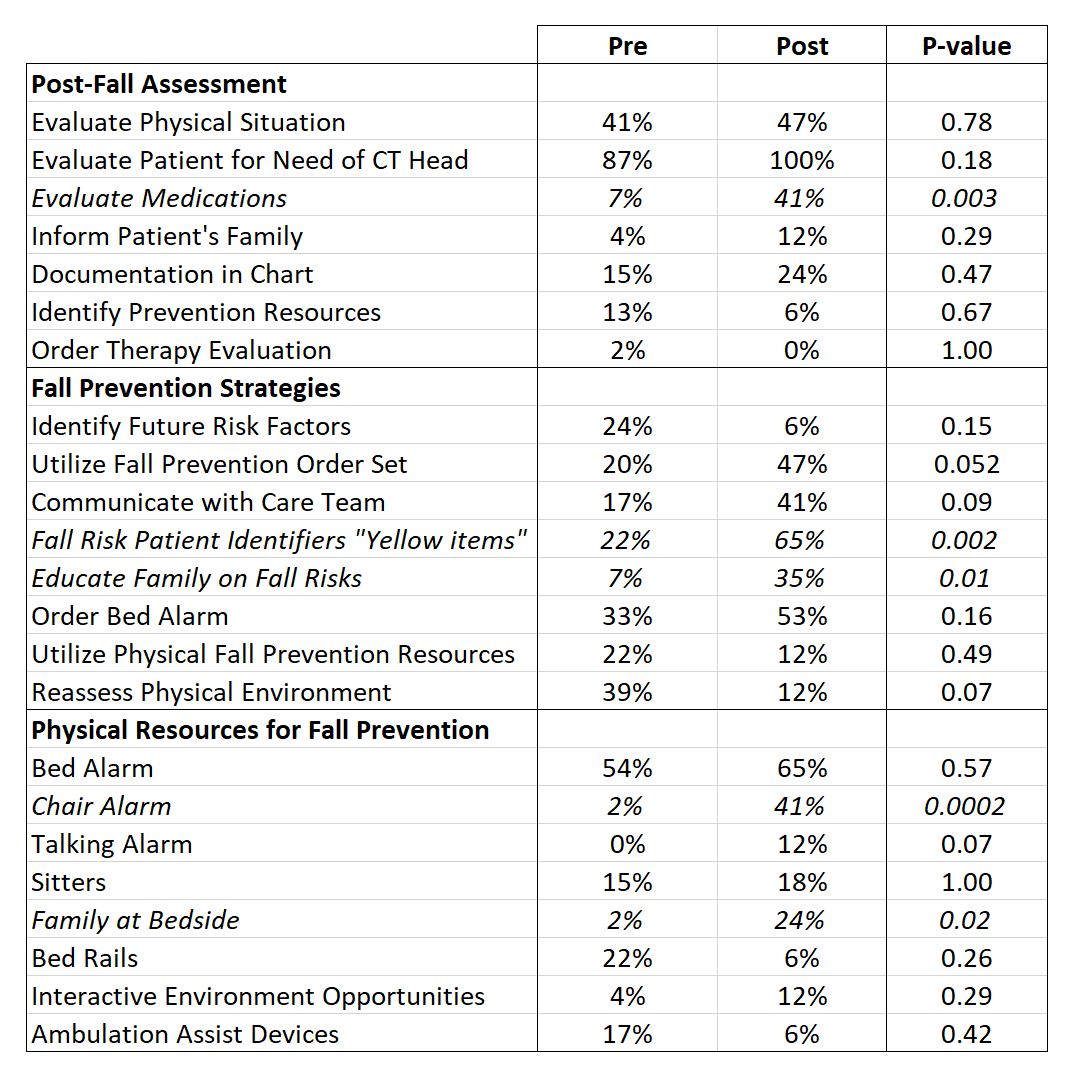
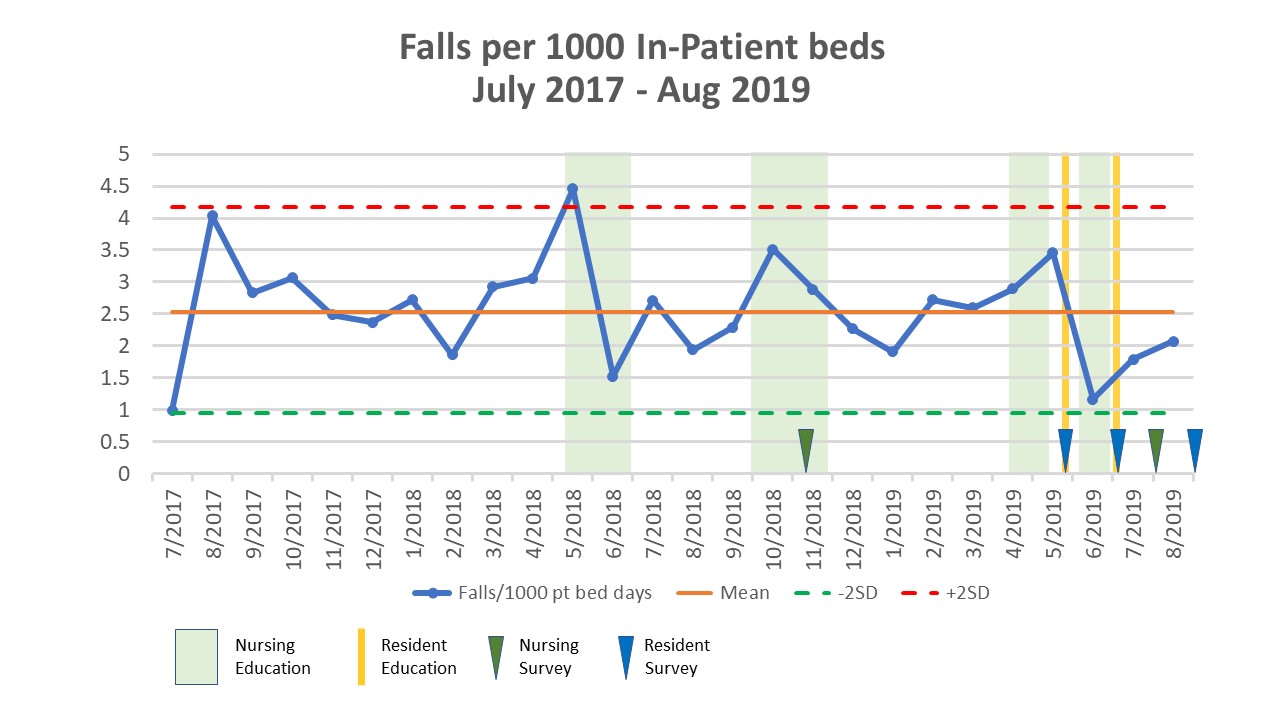
Results: A total of 46 residents completed the pre-intervention survey, 18 (39%) PGY-1s and 28 (61%) PGY2-3s. There were no significant differences in identification of risk factors, post-falls assessment protocol elements, identification of fall prevention orders within the admission order set, or additional resources for secondary fall prevention between the two groups, aside from post-fall communication (PGY-1 33% vs PGY2-3 7%, p=0.04). Post-intervention (Table 1), residents were significant more likely to know to complete a medication evaluation (7% vs 41 %, p=0.003). Residents were also significantly more likely to acknowledge physical fall-risk patient identifiers, “yellow items” (22 % vs 65%, p=0.002), identify chair alarms as a prevention resource (2% vs 41%, p=<0.001), and to educate family members on prevention strategies (7% vs 35%, p=0.01). Hospital fall rates were tracked over time and plotted in the annotated run chart of Figure 1, which also notes the dates of both nursing and resident education sessions.
Conclusions: Fall assessment and secondary prevention opportunities are not well known to Internal Medicine residents at the study institution. A focused educational sessions was able to significantly improve residents’ knowledge in multiple domains of post-fall evaluations and secondary prevention strategies, but did not alter the overall hospital fall rate.