Background: Diabetes affects 30.3 million people in the US, and 25% of total hospital days are incurred by patients with diabetes. Among hospitalized adults, diabetes is considered a chronic secondary diagnosis. As the population of patients with diabetes grows, so does the potential for adverse events during hospitalization. Previous studies have shown that both hyper- and hypoglycemia are associated with poor outcomes in broad populations of hospitalized patients, including increased morbidity and mortality. Hypoglycemia occurs in 3.5-10.5% of patients on the general medical floors and in 12-18% among patients with diabetes, owing in part to focus on glycemic control in patients with diabetes. Moderate glycemic control prevents microvascular complications and may reduce long-term cardiovascular complications; however, results from the ACCORD trial have shown that very intensive glycemic control may increase risk of mortality. Risk of hypoglycemia is especially pronounced in elderly patients with advanced duration of diabetes. As the population of adults with diabetes continues to expand, emphasis should be placed on identifying patients at risk for hypoglycemia and individualizing treatment strategies and glycemic targets to avoid adverse outcomes. We sought to identify patients with hypoglycemia preceding acute clinical deterioration requiring urgent response by our institution’s Rapid Response Team (RRT), a multidisciplinary modality that aims to rapidly assess, monitor, and reverse clinical deterioration.
Methods: We performed a retrospective chart review of three years of data acquired by our institution’s RRT. We identified 95 hospitalized patients who underwent a “rapid response” due to hypoglycemia (point-of-care capillary glucose or serum glucose <70 mg/dL). We performed a multivariate analysis to identify contributors to poor outcomes (defined as all-cause mortality) following a hypoglycemic event.
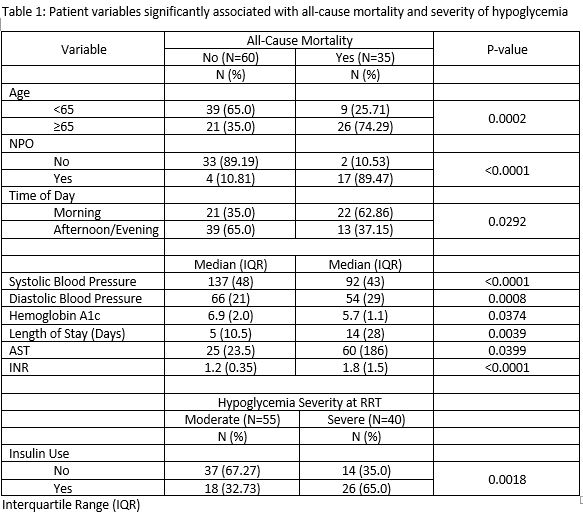
Results: Patients found to have significantly higher all-cause mortality following RRT for hypoglycemia (p< 0.05) were 65 years or older, had lower blood pressure, lower median hemoglobin A1c, longer hospital length of stay, were more likely to be NPO, and had a higher percentage of having an RRT in the morning. Patients who had a glucose level <41 mg/dL at time of RRT had higher rates of insulin use during admission when compared to individuals with higher glycemia.
Conclusions: As the diabetes epidemic worsens and more patients are hospitalized with the disease, it is critical that clinicians identify and manage risk factors for hypoglycemia. Our study identified several risk factors that were associated with all-cause mortality. Our findings support previous research that tight glycemic control can be detrimental to elderly patients . Based on our results, further research is needed to identify systems-based strategies for risk-stratification and prevention of inpatient hypoglycemia and improvement of patient safety.