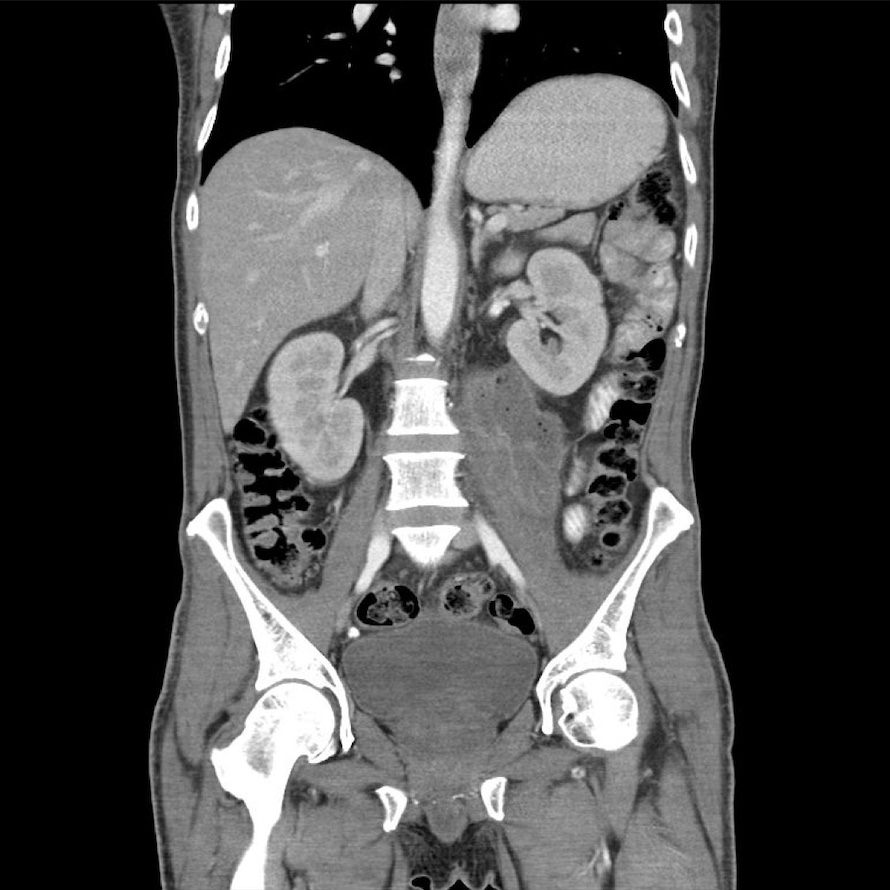
Case Presentation: A 49-year-old male with a medical history significant for unmanaged type 2 diabetes mellitus presented to the emergency department with generalized body weakness associated with 5 days of melena and coffee ground emesis in the setting of heavy use of naproxen for chronic severe lower back pain. He reported recent visits to a chiropractic clinic in Mexico, where he had undergone several epidural steroid injections. Physical examination revealed tenderness over the left flank with a limited range of motion due to severe pain. Vital signs showed tachycardia (heart rate: 128 bpm) and normal temperature (36.1°C). Laboratory investigations demonstrated leukocytosis (WBC count: 20,720 cells/mm³) with neutrophil predominance. Blood glucose was markedly elevated at 576 mg/dL. His diabetes was poorly controlled with an HbA1c level of 11.6% on admission. A contrast-enhanced CT scan of the abdomen and pelvis was performed, which revealed a 9 cm x 10cm x 4 cm complex mass involving the left retroperitoneal and left iliopsoas muscle consistent with an abscess, and bony erosion of the inferior endplate of L1. The diagnosis of the left iliopsoas abscess secondary to the recent epidural steroid injection was made. The patient was promptly started on empiric intravenous antibiotics with broad coverage: Piperacillin/Tazobactam and Linezolid and underwent image-guided percutaneous drainage of the abscess by interventional radiology. The patient showed significant clinical improvement following drainage and antibiotic therapy with a notable reduction in abscess on follow-up CT image and resolution of leukocytosis. On day 10 of admission, the final result of the culture obtained during drainage revealed Streptococcus constellatus, sensitive to Ceftriaxone. The antibiotics were changed to Ceftriaxone and Metronidazole to finish the 6-week course as an outpatient. Also, he was given extensive education on the management of diabetes mellitus type 2 and was initiated on insulin therapy, as well as close monitoring with a primary care physician.
Discussion: Infections are reported to occur in 1-2% of spinal injections, and severe infections are reported in 0.1-0.01% of cases. Iliopsoas abscess secondary to epidural steroid injection is rarely reported in the literature. The susceptibility to infection in patients with type 2 DM is known to be higher than in the general population. The possible mechanisms include the suppression of cytokine production, defects in phagocytosis, dysfunction of immune cells, and failure to kill microbial associated with the hyperglycemic state. In this patient, his type 2 DM was not well-managed with initial glucose at 576 mg/dL and HbA1c at 11.6%, which is thought to have contributed to a rare infectious complication from epidural steroid injection.
Conclusions: This case report illustrates the presentation, diagnosis, and management of a 49-year-old male with uncontrolled diabetes who developed a left psoas abscess subsequent to a recent epidural steroid injection performed at a chiropractic clinic. The diagnosis was confirmed via CT abdomen/pelvis, following which the patient underwent successful treatment involving percutaneous drainage and intravenous antibiotics. The case emphasizes the importance of considering infectious complications following epidural steroid injections, especially in patients with predisposing factors such as poorly controlled diabetes.