Background: Code status discussions and documentation are a key part of inpatient care for hospital medicine providers as they become more involved in caring for those with advanced illness. Hospitalists are challenged both with efficiently addressing a complicated subject due to time constraints and by a lack of established patient relationships. If it is not part of the patient care culture, the conversations are often not had or deferred until patients are no longer critically ill. We sought to push for a culture change to improve documentation of code status discussions amongst a hospitalist group.
Methods: A group of interested providers began to discuss barriers to discussions and documentation. Intentional, informal discussions between providers began in the provider workroom to bring awareness to the group. A formal presentation on tools to facilitate discussion and feedback regarding current practice was given. Residents and ICU providers did not receive the intervention.A random pre-intervention sample of patients from the Hospital Medicine Service (HMS) from January 1 to May 30, 2017, had their charts reviewed for presence of code status documentation. The History and Physicals, Discharge Summaries and key Progress Notes written by the primary team were reviewed. The training level and specialty of the documenting provider was recorded. A random post-intervention sample of encounters from March 26, 2018 to September 25, 2018, were reviewed in the same manner as the pre-intervention group. Data for demographics, Length of Stay (LOS), Encounter Type, ICU stay and Case-Mix Index (CMI) were pulled from the hospital’s Data Warehouse. These were then compared using Chi-Square and T-Tests.
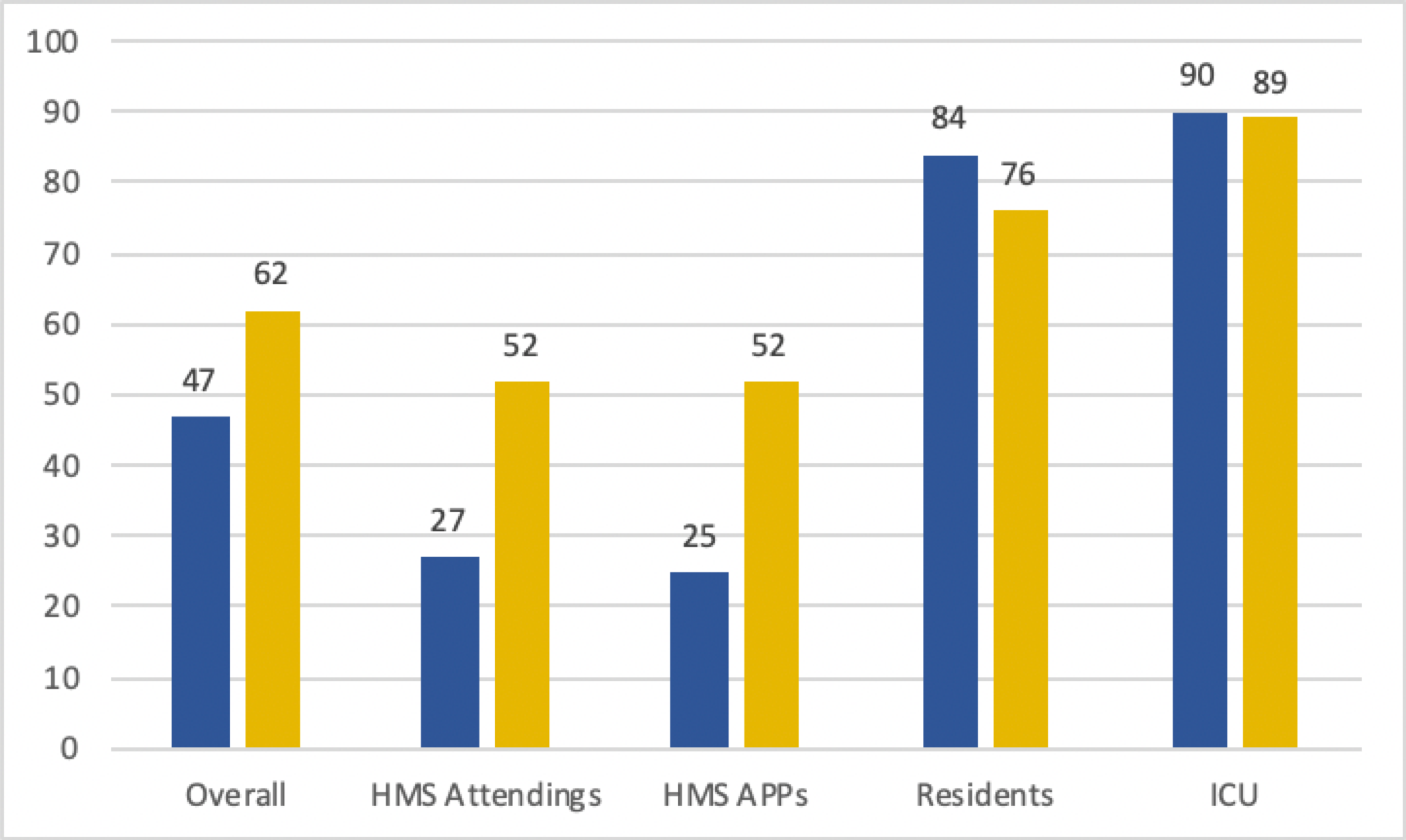
Results: 840 pre-intervention encounters were compared to 477 post-intervention encounters. The groups had no difference in ICU stay, Observation status, Age, Gender, Race, Palliative Care Consultation, Case-Mix Index, or Length of Stay. There was improvement in overall documentation 61% to 47% (p < 0.01). HMS Attendings improved from 27% to 52% (p < 0.01), HMS APPs improved from 25% to 52% (p = 0.01). There was a non-significant decrease in Resident documentation (84% to 76%, p = 0.17) and no change in ICU documentation (90% to 89%, p = 0.76).
Conclusions: Documentation of advance directives and code status remains a challenging component of patient care. This study demonstrates that the facilitation of a discussion on these topics and a dedicated group focusing on the issue can provide a culture shift that encourages providers to have these difficult conversations with more of their patients, and to document them in the EHR. Residents and ICU providers had a culture that was already firmly established and was maintained throughout the time period. Next steps of this study include continued educational interventions and evaluation of EHR tools to improve documentation practices by hospitalists.