Background: Chronic Obstructive Pulmonary Disease (COPD) is the 4th leading cause of death and a major driver of healthcare utilization worldwide. Established guidelines exist for hospitalized patients with COPD yet adherence to these has been found in multiple studies to be low. Our question is which Quality Improvement system changes best reduce healthcare utilization and improve adherence to COPD guidelines for patients hospitalized or at high risk for hospitalization for acutely exacerbated COPD (AECOPD)?
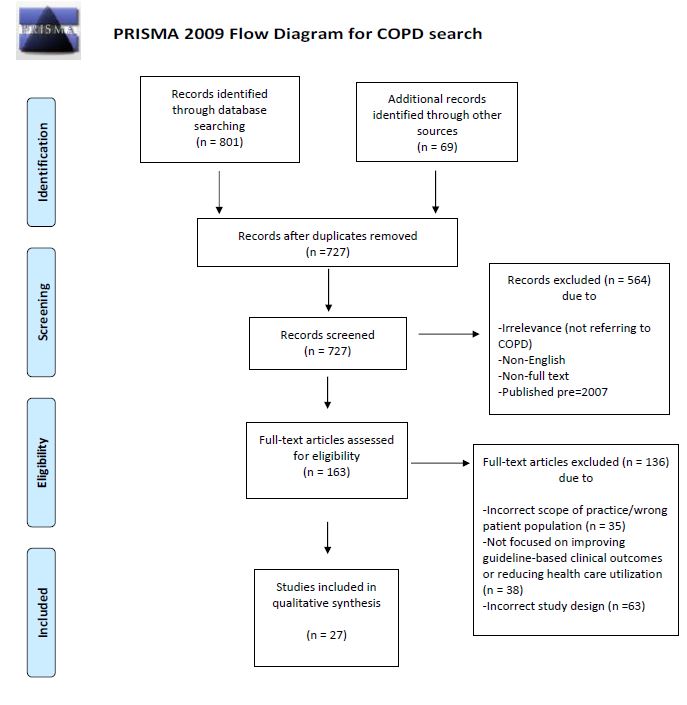
Methods: Search Strategy: Cochrane COPD Exacerbation trials, Medline (Jan 2007 to June 17th 2019), Embase (Jan 2007 to Oct. 4th 2019) and the references of relevant articles were reviewed.Selection Criteria: Included studies were full text, English randomized controlled trials (RCTs), non-randomized trials or prospective observational studies evaluating systems-based interventions to reduce hospitalizations, readmissions or acute care visits for AECOPD, to improve adherence to COPD guidelines or to improve mortality. Systematic reviews or retrospective studies were included at initial screening, but not in the final review.Data Collection: Full text articles were divided for data extraction and quality assessment, which was done according to the Delphi list and PRISMA guidelines. The lead author completed a final review.
Results: Twenty-seven articles were included for final review. Significant heterogeneity precluded formal meta-analysis. Trials were divided among two domains.Fifteen articles, involving 4,186 patients, focused on hospital-based interventions for patients with AECOPD. Four studied discharge bundles. These were mostly low-to-moderate quality studies with mixed results. Two showed decreased utilization. One showed improved guideline adherence, and the other found no difference. Eight mostly moderate-to-high quality studies examined inpatient ordersets with one also including a discharge bundle. All found significantly improved adherence to guidelines, but only one moderate-quality RCT reduced healthcare utilization. Three similar RCTs randomized 107 hospitalized patients to pulmonary rehabilitation (PR) post-discharge, but only one moderate-quality RCT showed significantly reduced utilization.Twelve studies evaluated 3,180 patients and reviewed comprehensive care management plans (CCMPs) with mixed results. Most involved an interdisciplinary COPD management team, providing intensive outpatient management and home action plans for self-management of symptoms. Seven, including one large, high-quality RCT which randomized patients to an intensive outpatient management program and one high-quality RCT which prioritized PR referral, showed significantly reduced healthcare utilization. One of these was stopped early due to a non-significant trend towards increased mortality. Three studies showed no difference in utilization, but two were low-quality, and the other was limited by a 58% dropout rate in the CCMP group. One moderate-quality RCT found increased healthcare utilization in the CCMP group. Lastly, a large, high-quality multi-center RCT was stopped due to increased mortality in the intervention group (28 vs 10, p-value = 0.003).
Conclusions: Inpatient ordersets and discharge bundles can improve guideline adherence for hospitalized patients with AECOPD, but CCMPs provide stronger benefit to reduce healthcare utilization in high-risk patients with COPD. Yet some concern remains that CCMPs may paradoxically worsen mortality.