Background: Recent Center for Medicare and Medicaid Services (CMS) rules require hospitals to have their physicians submit inpatient admission orders and certification prior to a patient’s discharge in order to justify hospitalization reimbursement; however, CMS does not specify how hospitals are to achieve this regulation. Use of Health Information Technology (HIT) tools has significantly expanded, have been shown to assist in meeting federal quality measures, and could be used to quickly assist a hospital in compliance with these federal regulations.
Purpose: To evaluate the impact of an HIT tool on CMS inpatient certification compliance at a tertiary academic medical center
Description: In this institutional review board-approved, prospective, interventional study over 12 months at a 793 bed tertiary academic medical center, we evaluated the impact of an HIT tool on compliance with CMS inpatient certification regulations. The HIT tool was implemented on the day the CMS rule went into effect and automatically created electronic physician inpatient orders and certification documentation for attending physicians whose Medicare patients were given an inpatient status. Physicians would receive an email from administrators with a web-based link for signature of orders they achieved with a confirmatory click. Administrators received real-time order and signature information for all qualifying patients and orders. Primary outcome was overall physician compliance with CMS regulations. Secondary outcomes evaluated the hospital medicine division and its compliance with the regulation, orders signed after discharge, and variation amongst its providers. Statistical analysis was performed with linear trend and chi-square test analysis.
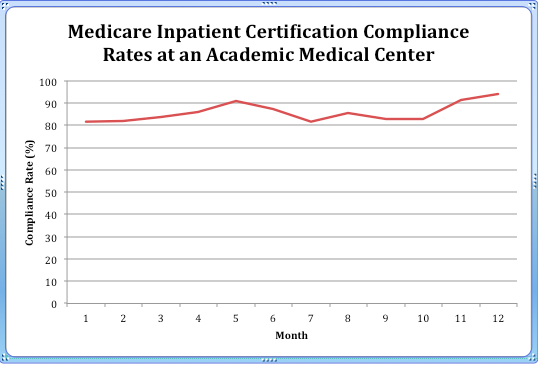
During the study period (October 1, 2013 to September 30, 2014), results showed over 12,449 inpatient admission orders and certifications created and a physician compliance rate of signing these prior to discharge of 86% (10,728/12,449) hospital-wide. 11% (1389/12,449) were signed after discharge, and 3% (381/12,449) were never signed or cancelled. Linear trend analyses demonstrated stable compliance with the measure with improvements seen with additional administrative interventions around education and additional administrative emails prior to discharge (p=0.62; Figure 1). The hospital medicine division composed of 43 providers of varying FTEs demonstrated a statistically significant difference amongst providers (p<0.05) with an overall compliance rate of 80.4% (1539/1914) with an additional 14.2% (271/1914) of orders that were signed after the patient was discharged, and 5.4% (104/1914) of orders that were never signed.
Conclusions: HIT tools can be quickly adopted and sustained to meet federal regulations for inpatient admission, but additional administrative oversight and interventions can assist in their optimization.