Background:
Code Blue events, or in-hospital patient emergencies, often require advanced cardiac life support (ACLS) and unfortunately can end in loss of life. Defining and measuring outcomes is an essential step for improvement in any process, but especially for a process as critical as Code Blues. In our institution, Code Blues are run by a multi-disciplinary team of providers, led by Internal Medicine senior residents. Previously, Code Blues were being recorded on paper sheets with no overall data collection process that provided for only minimal means of review. Without baseline information, it was difficult to monitor outcomes and Code Blue team process changes. We sought to implement a clearly defined method of Code Blue data tracking.
Purpose:
The primary aim of our project is to initially establish a baseline rate of Code Blue survival to the end of the event and to discharge. The secondary aim of the project is to identify areas for change in an effort to improve patient safety.
Description:
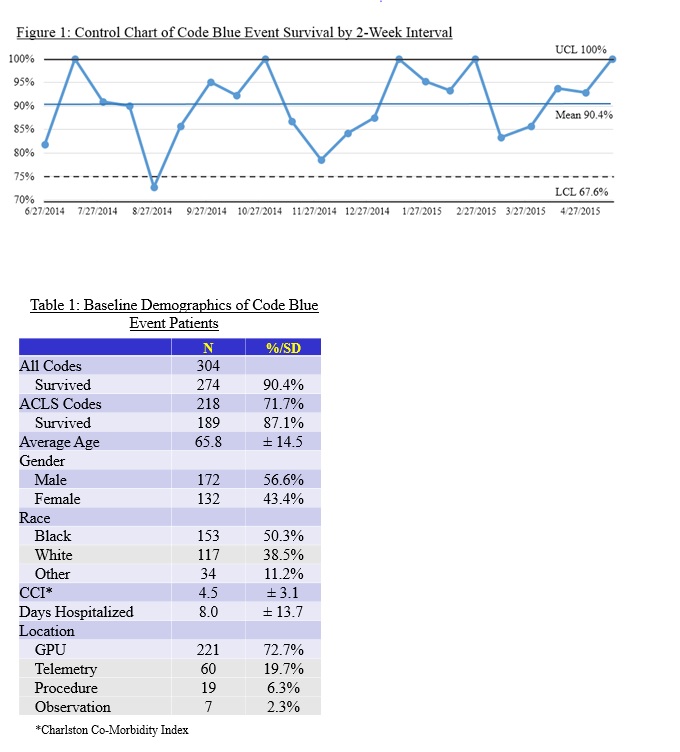
Our institution is an 800-bed urban tertiary referral center with a large Internal Medicine residency program. The Code Blue tracking started via a web-based data collection sheet run by the Chief Medical Residents (CMRs). After each Code Blue, the resident leader was required to fill out the tracking forms on an internal website. The tracking forms included code location, reason for decompensation, outcome, and an opportunity to note strengths and weaknesses of the event. The form was initially deployed to facilitate debriefing sessions after each. CMRs reviewed each form and compared with the Rapid Response team’s hand written worksheets every month to ensure completion. Large group debriefing meetings were held to review group data from the past month and to evaluate longitudinally for the year to date. Providers from other disciplines, including nursing, pharmacy, and administration were invited to attend and participate in the review and discussion. Initially, frequent feedback was required to residents to complete the form, but after 1-2 months it became a routine practice. After a year of data collection, we have been able to establish a baseline survival rate for events, displayed as a control chart in Figure 1. A total of 304 events were tracked, with demographics displayed in Table 1. Survival for all Code Blues was 90.4% and 87.1% for ACLS events. We were also able to identify potential improvements from the large debriefings, such as providing elevator keys for team leaders, crash cart medication reminders, and review of procedures for critical patient monitoring.
Conclusions:
An established baseline for Code Blue outcomes has allowed our institution to design process changes and accurately evaluate for improvement. Implementation of the tracking system was relatively smooth when its workflow was integrated into a key part of the post-event period, such as the debriefing process. Since our baseline survival rate is at or better than published rates, we have started to focus on process steps, such as communication with patient families during the event.