Background: Opioid use disorder (OUD) is a highly prevalent medical condition that is associated with significant morbidity and mortality. As rates of opioid addiction have increased in the last several years, hospitalists are uniquely positioned at the front lines to initiate evidence-based treatment for patients who are admitted with comorbid OUD and help link patients to outpatient care on discharge. However, despite this, many patients fail to receive appropriate treatment for their acute withdrawal symptoms and underlying addiction while hospitalized. At our 600-bed urban academic medical center, internal survey data shows that a majority of hospitalists lack the knowledge and comfort to adequately provide evidence-based medication assisted treatment (MAT) for opioid use disorder. Addiction consultation services that provide assistance in management of inpatients with substance use disorders, while effective, remain a limited resource at many acute-care facilities.
Purpose: We created a hospitalist-run peer support hotline to assist hospital medicine providers with opioid use disorder management in the inpatient setting.
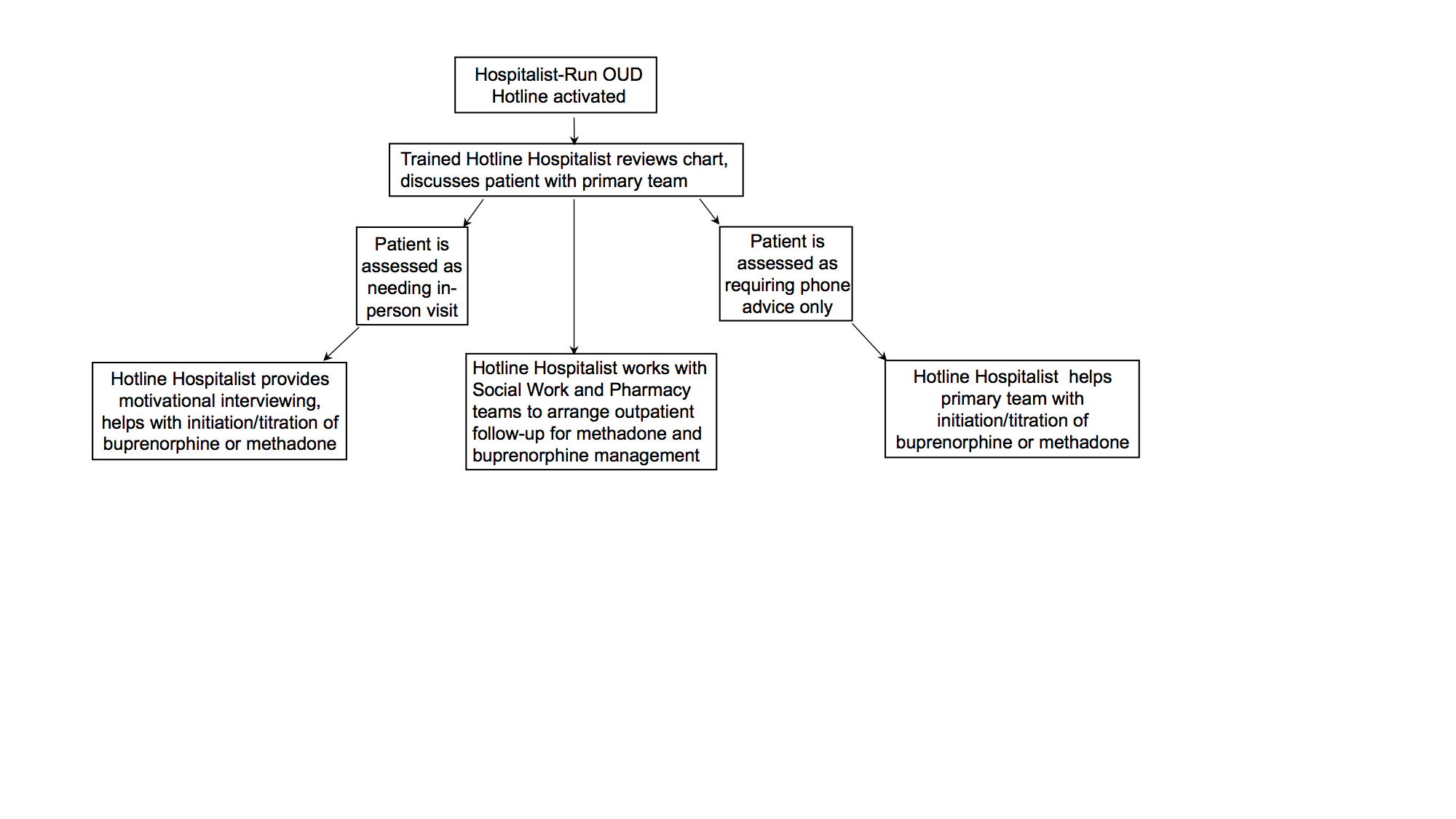
Description: We implemented a hotline for inpatient management of OUD which was staffed on a volunteer basis by hospitalists. Hospitalists staffing the hotline received eight-hour DEA-X waiver training coupled with eight hours of small group seminars on management of substance use disorders. The hotline (Figure 1) was active during daily business hours and helped inpatient medicine teams to address the following four questions: 1) Should my patient be started on Medication Assisted Treatment for Opioid Use Disorder? 2) Is buprenorphine or methadone more appropriate for my patient? 3) What is the clinical protocol for inducing/maintaining my patient on buprenorphine or methadone? 4) How do I arrange follow-up for my patient who has been started on Medication Assisted Treatment for Opioid Use Disorder? During the period between October 2018 and November 2019, our hotline services were activated in 72 patients, with 38 of these patients receiving an in-person visit by the hotline hospitalist. In the remaining 34 patients, the hotline hospitalist advised the primary service over the phone without seeing the patient in person. Demographically, 21 of the 72 patients were women, 51 were male, and 41 of the 72 patients were affected by housing insecurity. Of the 72 patients who received services, 61 were started or continued on buprenorphine or methadone. 68 of the 72 patients were offered a linkage to an outpatient MAT clinic or a residential facility capable of administering MAT.
Conclusions: This intervention demonstrates that a hospitalist-run hotline for inpatient management of opioid use disorder is a successful approach to leveraging hospitalization for the identification of patients with opioid use disorder and initiating evidence-based medication assisted treatment without requiring formal addiction medicine consultation.