Background:
Pay-for-performance incentives allow for engagement and motivation of participating physicians. Hospitalist compensation structure commonly combines base salary with performance and/or productivity-based incentives. Frequently used quality measures are value based purchasing metrics, patient satisfaction scores, adherence to guidelines and quality of medical documentation. Selection of metrics is strongly influenced by what is measurable and available. Hospitalists are ideally positioned to identify quality improvement (QI) projects, and therefore deliver high value patient care.
Purpose:
The objective of the program was to develop and implement a pay-for-performance structure focused on a successfully completed QI project.
Description:
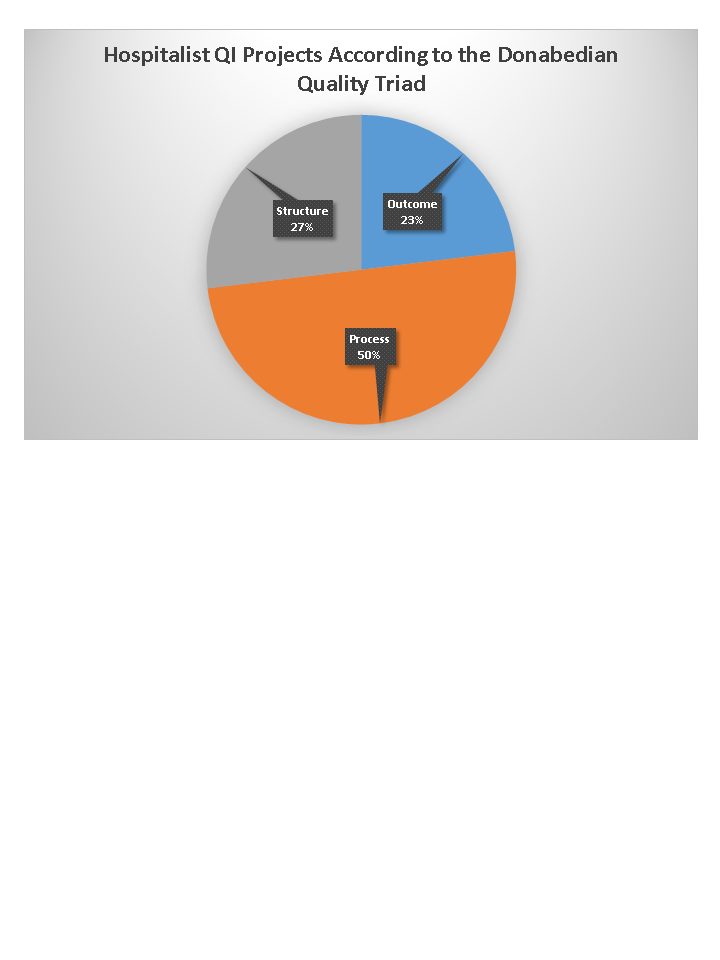
In January 2014, we collaborated with institutional stakeholders including quality, financial and legal leadership and identified a solution to transform the traditional QI project concept into a QI pay-for-performance incentive. The program was implemented in a large academic hospital with the Hospitalist Leadership overseeing the QI projects. In our group of 34 physicians, all full-time and part-time hospitalists were eligible to participate. The pay-for-performance structure consisted of 3 milestones. In the first step, we met individually with each hospitalist to identify eligible QI projects. Specifically, we focused on the following selection criteria: research topic relevance, feasibility of measurement with electronic health record data, alignment with institutional value and educational importance. The second milestone was centered on data analysis and third on project presentation. At each milestone participants were expected to meet with the Hospitalist Leadership to discuss their progress. We determined the financial incentive according to the number of milestones reached. Physicians were allowed to collaborate on large projects (e.g. readmission analysis, utilization of the medical crisis team). Thirty-two hospitalists, working on 27 projects, completed all milestones by the end of August 2015. Fifty percent of the projects focused on a process. All participants had the opportunity to present their findings to department and hospital leadership with 81% presenting in two large Hospitalist Quality Sessions organized in May and June 2015. During following academic year, several participants have used the QI project as a platform for advanced academic projects. In addition, this incentive program was extended to our first hospitalist community site.
Conclusions:
Completed quality improvement projects as pay-for-performance measures add value to the physicians, the hospitalist program, and the hospital system. Such incentive programs are feasible in both academic and community hospital-based practices.