Background:
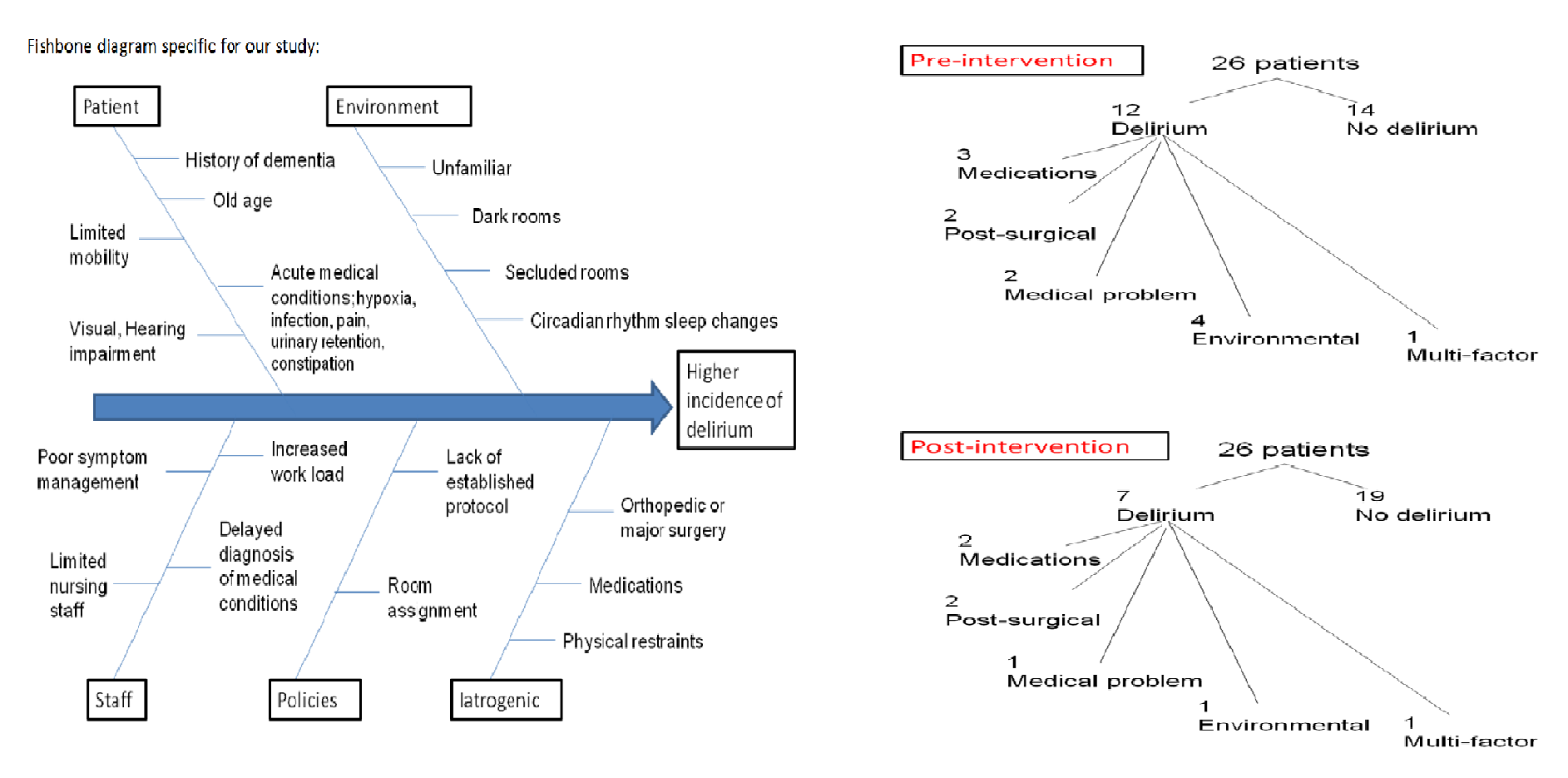
Delirium is an acute decline in attention and cognition that is potentially preventable among elderly population. Occurrence of delirium is followed by a sequence of events including loss of independence, increased risk of morbidity and mortality and increased health care costs. Development of delirium involves an interrelationship between vulnerable patients (with predisposing factors) and precipitating factors as illustrated in the fishbone diagram. Knowing these factors help clinician early identify at-risk patients to decrease chances of its occurrence as preventing delirium is the most effective strategy for reducing its frequency.
Methods:
In 2015, a pilot project was conducted at Robert Packer Hospital from February 10th to March 5th. This included elderly post-orthopedic surgery patients (elderly was defined as 60 years of age and over for this project) and patients with dementia at base line cognitive function on admission.
Patients with delirium at the time of admission and patients admitted to ICU were excluded from the study. Twenty-six patients with the aforementioned criteria were screened. Their identifiable information was not used for this project. In the pre-intervention group, nurses and residents responsible for these patients were interviewed on day 3 of the patients’ stay and were asked to complete a Confusion Assessment Method (CAM) questionnaire.
In the post intervention group, nurses and residents responsible for the enrolled patients were provided education, at the time of admission, about the non pharmacologic tools that were proven nationwide to decrease the incidence of delirium. We focused on managing 5 risk factors; cognitive impairment, sleep deprivation, immobility, visual/hearing impairment and medications.
These tools included:
- Orientation protocols as provision of clocks and blinds to help restore circadian balance
- Cognitive stimulation and encouraging regular visits from family and friends
- Facilitation of physiologic sleep with avoidance of interruption during sleeping hours
- Early mobilization and minimized use of physical restraints
- Patients with visual or hearing impairment were motivated to use their glasses and hearing aids.
- Monitoring the use of medications that are commonly implicated in precipitating delirium as benzodiazepines or opioids
Various approaches for interventions including educating residents, educating nursing staffs and sending electronic reminders to the residents were done.
After this intervention, the nurses and residents were administered the CAM questionnaire on the third day of the patients’ stay. Pre and post intervention data was gathered.
Results:
Pre-intervention group, 12 out of 26 patients were found to have delirium (48%) with different precipitating factors. Post-intervention group, 7 out of 26 patients were found to have delirium so the incidence has decreased to 26.9 %
Conclusions:
This project was undertaken to increase the awareness on a non costly, easy and available intervention to prevent delirium. Post intervention study showed that the incidence of delirium has significantly decreased. However, there is still a considerable percentage that could be prevented and in order to achieve this, we propose that these familiar practices should be a mandatory process or a reminder to be done in electronic health records. Also, education of providers and nursing staff must be an ongoing process. This will help reduce the incidence of delirium with its deleterious sequelae.