Background: Severe alcohol withdrawal and delirium tremens (DTs) are challenging therapeutic dilemmas. To prevent complications and death, management requires close monitoring and intensive treatment, frequently in an ICU. Benzodiazepines are first line therapeutic agents, but optimal use and dosing has been limited, due to a lack of randomized double-blind trials. In lower acuity patients admitted to a detoxification unit, systematic symptom-triggered benzodiazepine therapy (STT) has been established to be more effective than fixed-schedule (FS) dosing with episodic STT. Patients treated using STT require lower total benzodiazepine dosing and achieve shorter treatment durations. However, in higher acuity patients admitted to general medical services, retrospective analyses have not shown an advantage of STT over FS and STT. The purpose of this study is to determine if STT is more effective than FS with episodic STT in the management of high acuity alcohol withdrawal patients.
Methods: Two study groups were identified: a pre-intervention group consisting of 80 consecutive admissions prior to July 2017, and a post-intervention group consisting of 80 consecutive admissions after October 2017. In the pre-intervention group, patients were treated based on physician preference consisting of a fixed dose regimen with additional doses as needed. In the post-intervention group, providers were instructed to utilize STT protocol. The STT protocol allowed for escalating doses for higher withdrawal scores. During each period, adult patients (18 and over) admitted or transferred to a medical step down unit with ICD-10 defined primary or secondary alcohol withdrawal diagnoses, were evaluated. Patients were excluded from evaluation if they were transferred to the step down unit after seven or more days in the hospital, were chronically on benzodiazepine therapy, had left the hospital against medical advice during treatment, or if they had stayed over 30 days.The primary outcome measure was total lorazepam-equivalent dose of benzodiazepines. Secondary measures included average length of stay, seizure incidence, DT incidence, sitter use, behavioral emergency responses, leaving against medical advice, intubation, transfer to ICU, and death.
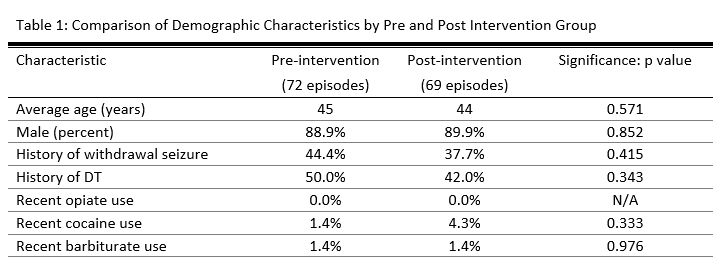
Results: 72 episodes during the pre-intervention and 69 episodes during the post-intervention period met inclusion criteria. 8 pre-intervention episodes were excluded because the patient left against medical advice (AMA). 11 post-intervention episodes were excluded- 9 episodes were due to patient leaving AMA, 1 due to chronic benzodiazepine usage and 1 due to transfer to step down unit after 7 days. Baseline characteristics of the pre- and post-intervention group were similar in Table 1. Implementation of the intervention was associated with a significant reduction in average (per patient) cumulative benzodiazepine dose, from 250 mg to 96 mg (p<0.001). Average length of stay decreased from 8.0 days to 5.1 days (p<0.001). Secondary safety measures were notable for a reduction of delirium tremens from 47.5% to 22.5% (p<0.001) and reduction of patients getting intubated from 13.8% down to 1.3% (p=0.003).
Conclusions: STT protocol appears to be more efficacious in treating severe alcohol withdrawal patients than a STT+FS protocol as evidenced by reduction in benzodiazepine usage and reduction in ALOS. STT protocol has also proven to be safer as fewer patients develop delirium tremens and fewer patients get intubated.