Background: Clinical documentation is essential for adequate representation of patient quality care metrics and accurate diagnosis capture but rarely taught in graduate medical education. Inaccurate capture of diagnoses leads to clinical documentation integrity (CDI) queries, which increase workload on busy providers. Implementation of a standardized note template for our resident physicians previously resulted in an increase in average diagnosis codes (18 to 19.5), CC/MCC capture rates (71% to 74%), and Elixhauser comorbidities (3.8 to 4.5) as well as decrease in CDI queries (46% to 30%). There was overwhelming agreement (>95% of resident survey responses) that the note template allowed for more conference attendance and timelier sign out (1).We aimed to further improve, simplify, and standardize diagnosis documentation via embedding a common diagnosis menu within the electronic health record (EHR) note template and assessed whether there was an increase in billing accuracy and overall decrease in CDI queries on our inpatient internal medicine teaching services.
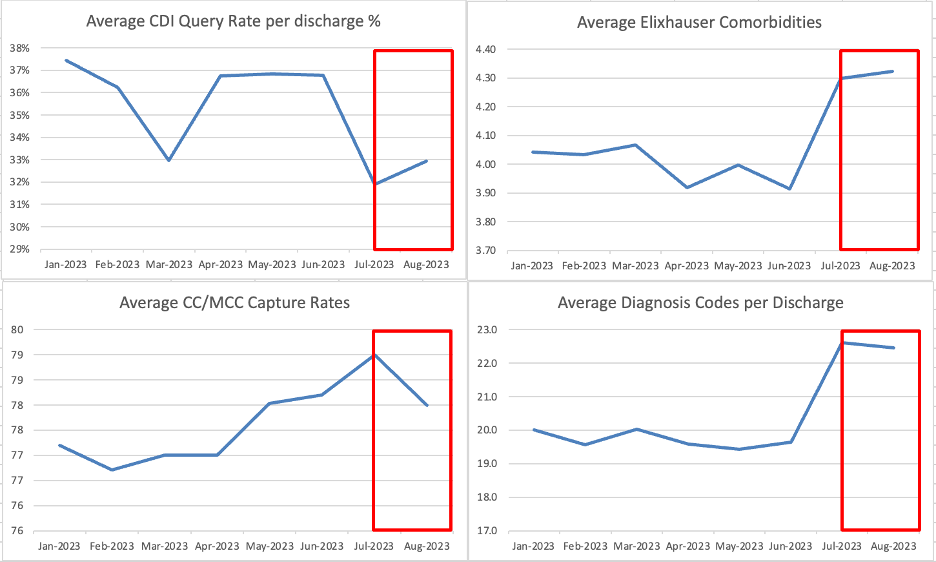
Purpose: For the initial pilot study, a standardized, common diagnosis menu in congruence with clinical billing codes was developed for the general internal medicine teaching services between the months of July 2023-Aug 2023 and placed within the admitting note template. Residents were surveyed post-implementation to assess the utility and ease of use of this interactive template. Free-text survey responses were included to evaluate if residents preferred inclusion of additional diagnoses.Measures pulled from Epic 6 months pre-, and 2 months post-template implementation included clinical documentation integrity (CDI) queries, average diagnosis codes per discharge, complication or comorbidity (CC) or major complication or comorbidity (MCC) capture rates, and average Elixhauser comorbidities. Mean pre-and post-template values will be calculated in the future via statistical process control (SPC) chart analysis.
Description: In the post-implementation survey, there was a 45% response rate from internal medicine residents, the majority of which reported that expanding the common diagnosis list would be useful (83%), and 42% of residents reported that this intervention saved them time when admitting patients. There was an overall decrease in CDI query rate (36% to 32%), slight increase in CC/MCC capture rates (77 to 78), increase in Elixhauser comorbidities (3.9 to 4.3, and increase in average diagnosis codes (19.7 to 22.5).
Conclusions: The implementation of a standardized diagnosis menu based on clinical billing codes is an effective way to improve quality metrics including accurate diagnosis capture, as well as reduce administrative burden by reduction of CDI queries. This menu also works as a real-time educational tool for resident teaching services. Given the success of this tool, we plan to increase the number of billable codes within the standardized menu as we continue to monitor these metrics.