Background: With the broad implementation of electronic health records, clinical documentation integrity continues to be under increasing scrutiny. On average, physicians spend over a third of their time documenting patient data¹; this burden has been extensively correlated to burnout². Leveraging automated note templates with integrated safety rounding checklists, we attempted to standardize more efficient documentation that allowed resident providers more time for educational activities and earlier end of day sign out while refining the documentation of medical comorbidities and safety checks.
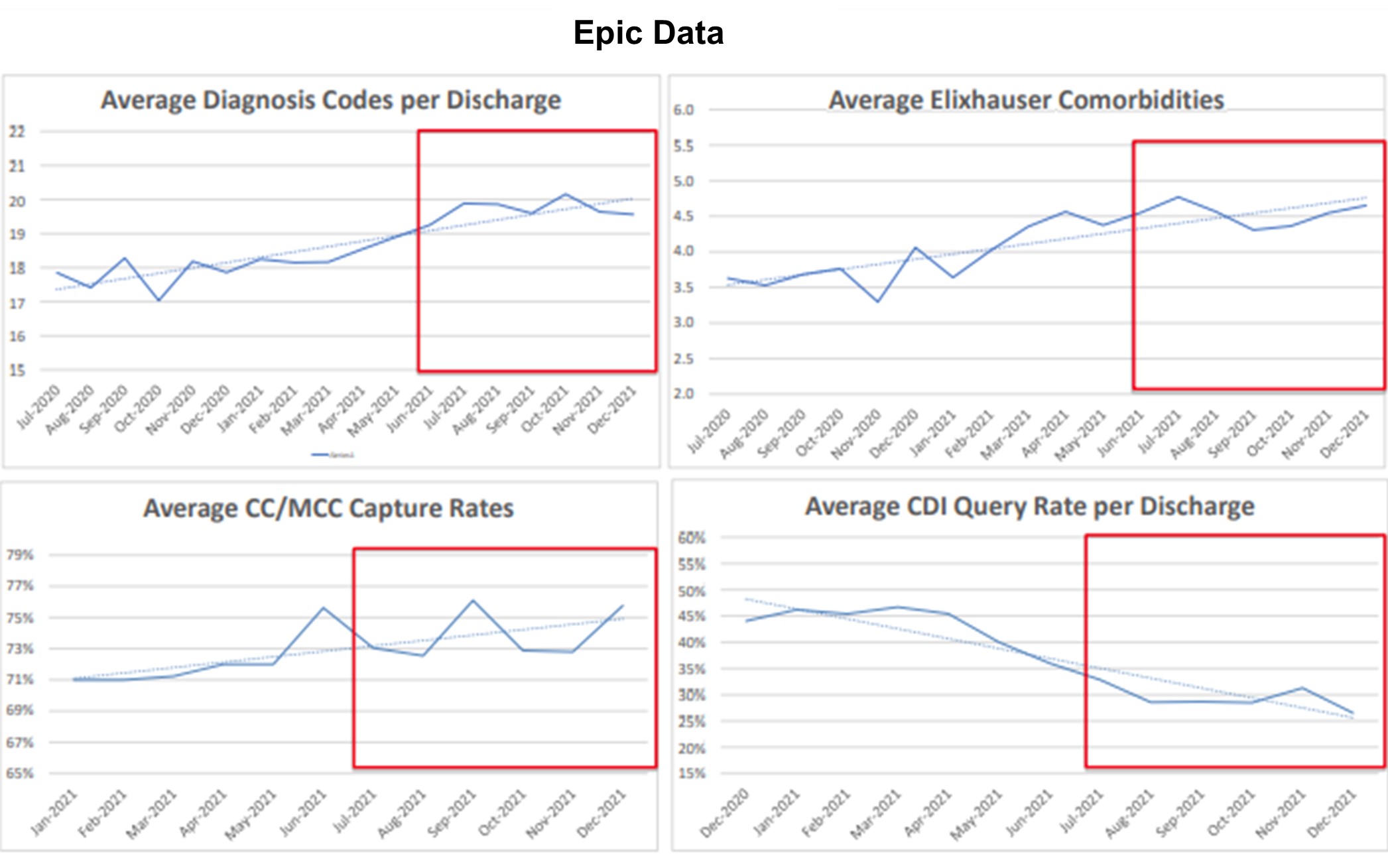
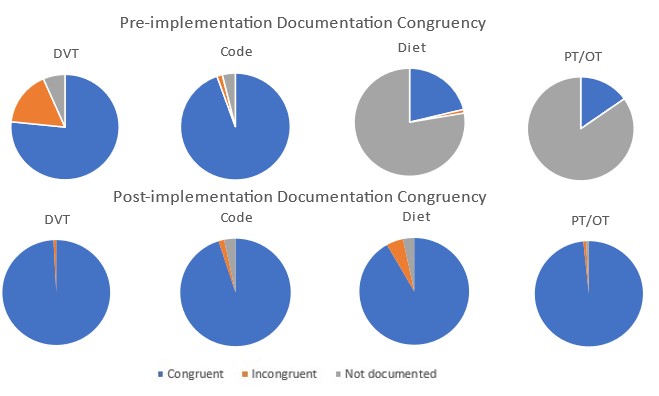
Methods: A standardized, automated note template was developed for the medicine teaching services that included forwarding of the assessment and plan and integrated disappearing “Help Texts” guiding proper documentation of diagnoses. Measures pulled from Epic 10 months pre- and 9 months post-template implementation included clinical documentation integrity (CDI) queries, average diagnosis codes per discharge, complication or comorbidity (CC) or major complication or comorbidity (MCC) capture rates, and Elixhauser Comorbidities. Mean pre-and post-template values were compared via Student’s t-Test. Residents were surveyed post-implementation to assess impact on perceived efficiency. Additional free-text survey responses prompted further updates to the template to include a safety rounding checklist that automatically incorporated a patient’s code status, deep venous thrombosis (DVT) prophylaxis, diet, and physical/occupational therapy (PT/OT) orders. Via manual chart review, we assessed these categories for congruency between active orders and documentation one month prior to and following the update.
Results: There were statistically significant increases (p< 0.01) in average diagnosis codes (18 to 19.5), CC/MCC capture rates (71% to 74%), and Elixhauser comorbidities (3.8 to 4.5) as well as decrease in CDI queries (46% to 30%). There was overwhelming agreement (>95% of resident survey responses) that the note template allowed for more conference attendance and timelier sign out. Following implementation of the safety rounding checklist, there was improved congruency between active orders and documentation across DVT prophylaxis (76.6% to 99.2%), code status (94.5% to 95.1%), diet (21.2% to 91.0%), and PT/OT (15.2% to 98.4%).
Conclusions: The electronic medical record can be effectively leveraged to improve documentation accuracy and efficiency. Residents agreed that the automated template saves time, allowing for better conference attendance and earlier sign out. Resident feedback drove significant improvements in documentation accuracy and continuous process improvement was vital for the success of this intervention.Documentation of diet orders and active therapies dramatically improved with an automated safety rounding checklist. Automatic incorporation of ordered DVT prophylaxis was coupled with a hard stop built into the note that forced residents to consider the appropriateness of the ordered DVT prophylaxis. While there was marked improvement in congruency between ordered and documented DVT prophylaxis, the clinical impact of the improvement is uncertain; potential areas for further investigation include examining in-hospital DVT rates, major bleeding events, and length of stay.