Background: Provider continuity can improve many aspects of an inpatient stay however, there is a lack of data on whether it could affect mechanical ventilation weaning. During the COVID-19 pandemic, many patients required tracheostomies and mechanical ventilation. This study evaluated whether provider continuity could increase mechanical ventilation weaning outcomes in the inpatient setting.
Methods: Data was collected retrospectively from April 2020 to May 2022 for patients admitted to the pulmonary stepdown unit (SDU) at Yale-New Haven Hospital. A new staffing model was started in February 2021 where a small group of physicians and advanced practice providers (APPs) continuously rotated through the unit. Ventilator weaning protocols were used before and after initiating the new staffing model.
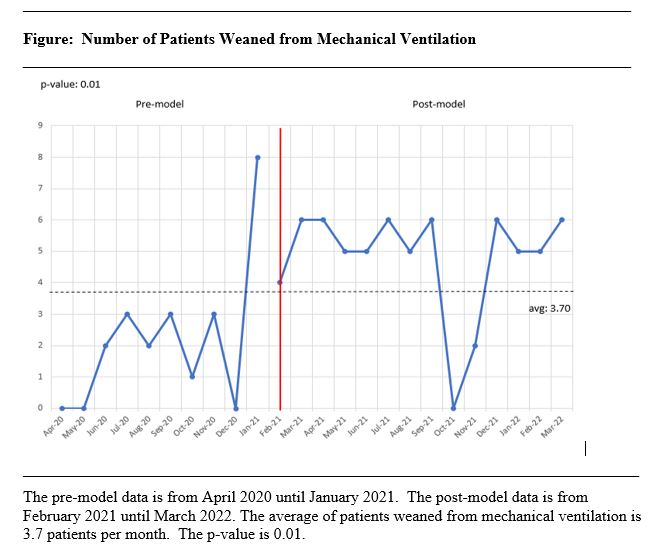
Results: A total of 185 patients were reviewed and included in the study. During the 2-year timeframe, 46% of the patients were weaned off the ventilator (n=86), with 26% of the patients weaned occurring prior to the staffing model (n=22) and 74% of patients weaned after the staffing model started (n=64). The mean number of patients weaned off the ventilator was 3.7 per month. The increase in patients weaned from the ventilator after the staffing model was statistically significant (p = 0.01).
Conclusions: There was a significant increase in mechanical ventilator weaning outcomes after initiating the new staffing model. This study shows how continuity of care can affect mechanical ventilation weaning in the inpatient setting.