Background: Sub-optimal communication during care transitions contributes to poor patient outcomes. Patients who undergo interhospital transfer (IHT, the transfer of patients between hospitals) are at especially high risk given their level of illness severity. In examination of the IHT process at Brigham and Women’s Hospital (BWH), a 740-bed tertiary care referral hospital, we previously found that patients transferred to the general medical service (GMS) arrive without advanced notification of the admitting provider over 35% of the time. Inadequate communication with frontline clinicians who assume care for IHT patients at time of arrival is a potential safety concern.
Purpose: To improve advanced notification of IHT patient arrivals on GMS for admitting providers.
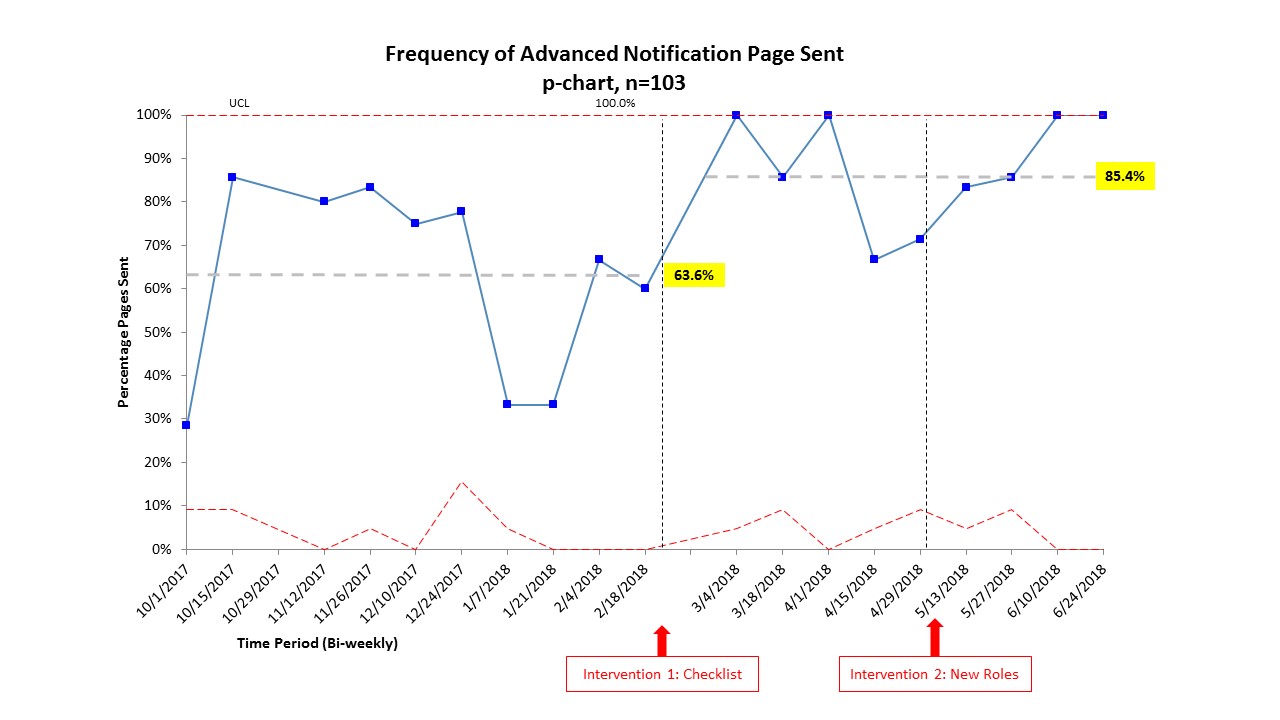
Description: We engaged a group of key stakeholders in IHT at BWH, including GMS physicians, the BWH Access Center responsible for coordinating all hospital transfers, and bed coordinator staff. Most frequent contributing factors leading to non-notification of the admitting provider were identified and quantified via process mapping and Pareto chart construction, and a priority/pay-off matrix of potential solutions was constructed and reviewed. Based on this analysis, we selected and implemented two high impact/low resource interventions: (1) A paper-based checklist for the bed coordinator to “Page the admitting provider” at the time of bed assignment of the transferred patient; and (2) Streamlining roles such that the bed coordinator (who assigns beds to transferred patients) assumed responsibility for paging the admitting provider. Education of the Access Center and bed coordinator staff regarding new roles and responsibilities was included with the intervention. Data on frequency of advanced notification pages was collected over 9 months, including 103 patients transferred to GMS during this time. We found that advanced notification of IHT patient arrivals to the admitting provider increased from a baseline of 63.6% to 85.4% following implementation of the two interventions (Figure).
Conclusions: Our interventions collectively improved advanced notification of IHT patient arrivals for admitting providers by 21.8%. Based on feedback from our group of stakeholders, the most successful components of the interventions included redesigning roles to streamline the IHT process, staff education, and using visual reminders (i.e., a checklist) for the paging task. We anticipate these improvements will lead to more timely treatment of IHT patients and may improve patient outcomes. We plan to disseminate this to include patient transfers to other services.