Background: Hospital medicine patients with complex behavioral and psychiatric needs benefit from specific resources and training. Inability to provide intensive, longitudinal, and specialized support for patients with psychiatric needs contributes to dissatisfaction in clinical work for hospitalists, and may increase the risk for workplace violence from patients. Little is known about the prevalence of psychiatric disease among hospital medicine patients and their inpatient care utilization. Our aims were to examine the prevalence of psychiatric disease among hospital medicine patients over time and use of a behavioral support program to inform future care delivery models that better meet the needs of patients and clinical teams.
Methods: In 2021, our institution started a Care Support team staffed by nurses who support patients and providers in trauma-informed care. To understand the need for resources and programmatic expansion, we analyzed electronic health record data for patients with psychiatric needs on the hospital medicine service at a 700-bed hospital in a large urban health system between January 2018 and December 2022. We used descriptive statistics to understand the proportion of hospital medicine patients on a psychiatric hold and their length of stay data relative to the overall hospital medicine population. For the 2 years after the inception of the Care Support team, we examined the number of patients who had both a psychiatric consult and a Care Support consult. A linear regression was performed to understand trends over time. We used a t-test to compare continuous variables and chi-square tests to compare categorical variables.
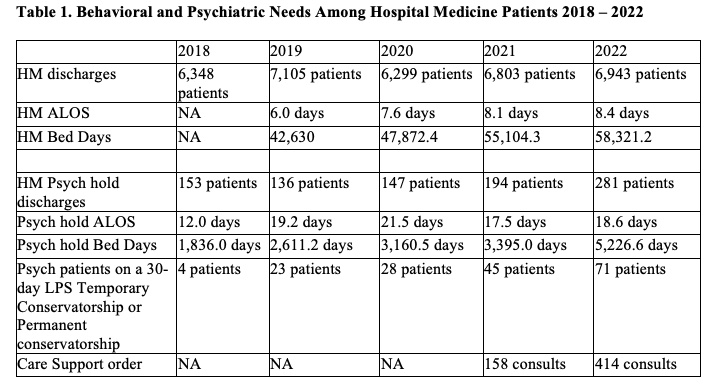
Results: We analyzed data from 33,498 discharges on the Hospital Medicine Service across 5 years (Table 1). Between 2018 to 2022, the number of hospital medicine patients on any psychiatric hold increased from 2.41% of discharged patients to 4.05% of discharged patients, a 60% relative increase (p< 0.001). The average length of stay (LOS) for hospital medicine patients with a psychiatric hold was significantly higher than the average LOS for all hospital medicine patients (19.2 vs 7.5 days; p< 0.001). The number of patients on a 30-day, temporary LPS Conservatorship, and Permanent conservatorship increased significantly (p=0.04). The number of patients with a Care Support consult significantly increased between 2021 and 2022 (p< 0.001). Among patients with a psychiatry consult, the number of Care Support consults significantly increased from 71 in 2021 to 166 in 2022 (p< 0.001). As a proportion of patients with a psychiatry consult, the share of patients who also received a Care Support consult increased from 2.8% in 2021 to 6.6% in 2022 (p=0.9).
Conclusions: Our study finds that the percentage of hospital medicine patients requiring a psychiatric hold and temporary or permanent conservatorship has significantly increased over time, along with the total bed days. Programs like the Care Support consult increased significantly, but the growth in this population has outpaced the team’s capacity. Future avenues to support this expanding population includes Care Support expansion, dedicated training for high volume units, and increased staffing for units with higher volumes of behaviorally complex patients.