Background: Avoiding preventable readmissions is a major goal of health care systems nationwide1. The Cardiorespiratory cohort consists of Veterans admitted with a diagnosis of CHF, COPD and non-COVID-19 Pneumonia, and is a high-risk group for readmissions. As part of a larger National VA High Reliability Organization (HRO) Collaborative2, an interdisciplinary team was launched to achieve a reduction in hospital-wide readmissions.
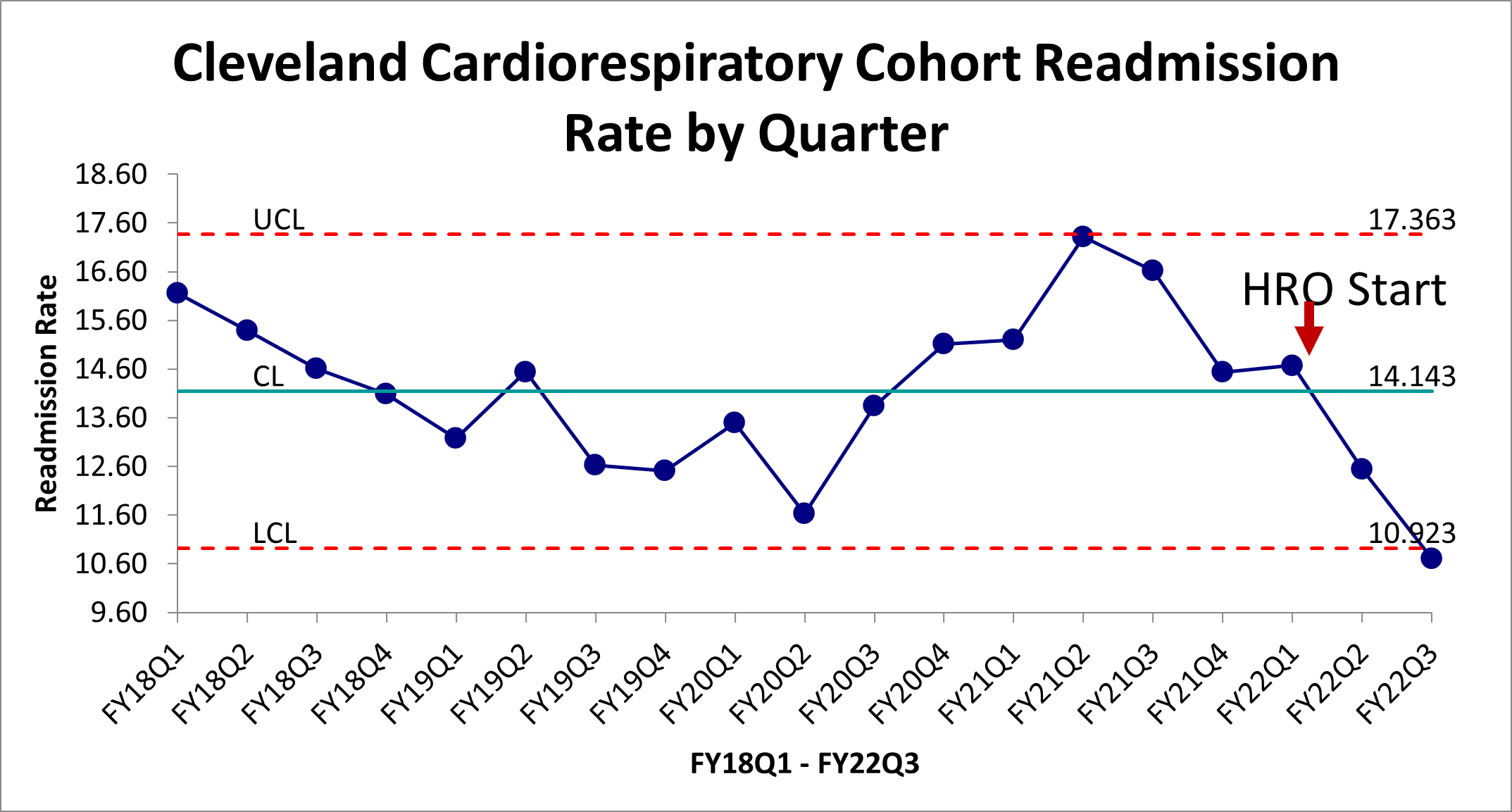
Purpose: The overall aim was to reduce hospital-wide 30-day readmission rate (HWR) for the Cardiorespiratory cohort at the Veterans Affairs Northeast Ohio Health System from a baseline of 14.55% to < 12% by the end of the Quarter 4 of the 2022 Fiscal Year.
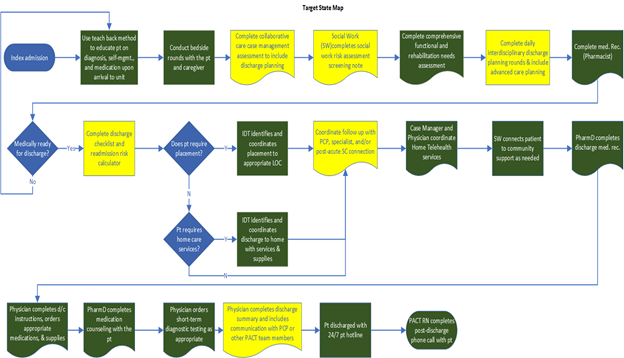
Description: Veterans were considered in-scope for readmissions for a cardiorespiratory diagnosis after index admission to acute care and out of scope if readmitted for anything other than a cardiorespiratory diagnosis, or admitted to medical observation, hospice, or the VA Community Living Center. Using the Lean Six Sigma A3 process, current and target state maps were identified after chart and literature review and the team chose to focus on increasing emphasis on patient communication and interdisciplinary collaboration, specifically during the time of transitions of care3-6. Stakeholders were interviewed via an extensive Gemba Walk as part of the Gap Analysis to generate a solutions approach. Following this, four rapid experiments were undertaken: 1) increasing use of the existing multidisciplinary Home Base Primary Care (HBPC) consultation service to perform prompt home visits for veterans in the Cardiorespiratory cohort with a high risk for readmission. The VA Care Assessment Needs (CAN)7 score was used as a risk stratification tool, and patients were eligible for the intervention if their CAN score was >/= 90. 2) two of the four primary hospital medicine teaching teams were instructed to invite patient caregivers to bedside walk rounds and to 3) write down the plan of care on the white board in the patients’ rooms and 4) a daily interdisciplinary team meeting was scheduled on the inpatient Cardiology service with a focus on transitions of care. In the first few weeks post-implementation, average consults per week to HBPC in this cohort increased 50%, however as the project continued, no significant increase in consults was noted. Fewer than 10% of patients had family invited to rounds and this piece of the initiative was abandoned after 4 weeks. Plans of care were written on the white board for 67% and 22% of the patients on the interventional inpatient teams. The outcome measure of readmissions in the cardiorespiratory cohort showed a significant reduction, from a baseline of 14.55% in quarter 4 of 2021, to 12.49% in the first quarter of the project, down to 10.9% in quarter 3 of 2022 after implementation of the above experiments. This was the lowest readmission rate in that cohort in at least 5 years and met statistical special cause variation. Quarter 4 data for 2022 is not yet available.
Conclusions: Overall, the commission of a large, multi-disciplinary team with a focus on reducing hospital-wide readmissions in the Cardiorespiratory cohort and their subsequent process improvement efforts was associated with a significant reduction in readmissions to historically low levels.