Background: Respiratory rate (RR) is a predictor of adverse outcomes and an integral component of many risk prediction scores for hospitalized adults. Despite its clinical value, RRs are often inaccurate and may lead to misclassification of disease severity, potentially jeopardizing patient safety.
Purpose: We sought to improve inpatient RR measurement by patient care assistants (PCAs) through a multipronged quality improvement (QI) initiative in a single inpatient unit of our large, urban safety-net hospital.
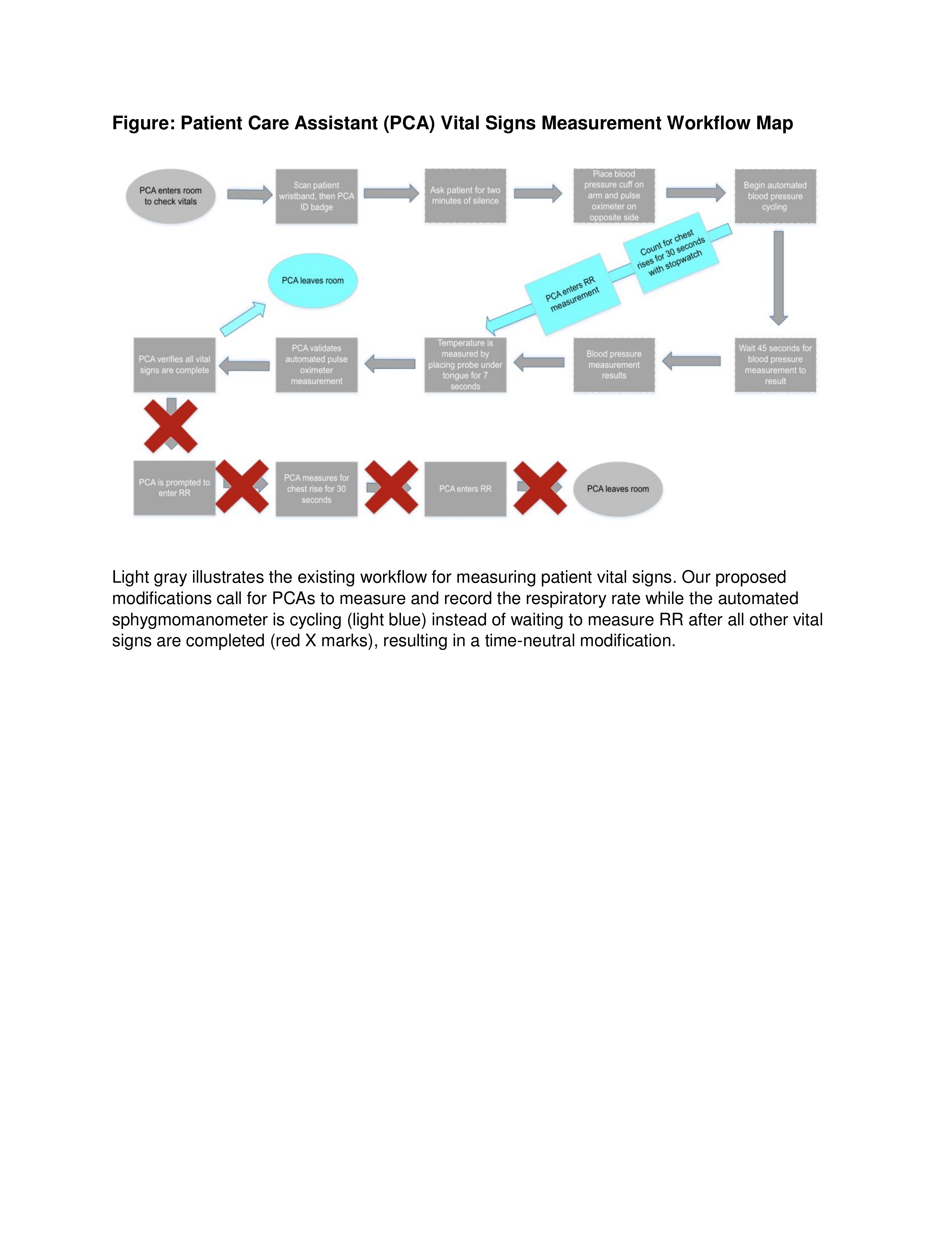
Description: We observed and mapped PCA vital sign measurement workflows to assess RR accuracy compared to a “gold-standard” measurement by trained study team members (NK, KB). The workflow took an average of 3 minutes (IQR 2–3.5), and the median ‘gold-standard’ RR was 16 (IQR 12–18) versus 18 (IQR 18–20) for PCAs with a mean difference of 4.4 (p<0.01). Only 36% of PCA-measured RRs were ‘accurate’, defined as being ±2 breaths per minute of the gold-standard RR. We identified 2 key logistical barriers to accurate RR measurement: absence of a time-keeping device and a perceived lack of time to measure RR, consistent with findings from prior studies. To address these barriers, we engaged key stakeholders including nursing operations management, nursing education leadership and hospital administration. Our intervention a) adds a time-keeping device to vitals carts; b) includes a time-neutral workflow modification calling for RR measurement (30 seconds) during automated blood pressure measurement (45 seconds; see Figure); c) implements RR measurement skill labs during new PCA orientation; d) retrains existing PCAs on RR measurement during monthly unit staff meetings and daily PCA & nursing huddles; e) implements regular, routine vital sign audits; and f) designates PCA ‘Vital Sign Champions’ to be local unit champions for cooperation, accomplishment, and excellence in vital sign measurement.
Conclusions: Through a continuous QI initiative, we hope to create a lasting culture change to overcome our collective long-standing complacency for human error in RR measurement to ultimately improve patient outcomes. In the upcoming two months, we plan to evaluate RR accuracy and time spent on vital sign measurement after full implementation of our modified workflow.