Background: What happens when “best practice” is not practiced? Prescribing naloxone to patients at high risk of opioid overdose is considered best practice by the United States Department of Health in order to decrease the risk of overdose and maximize patient safety. Research also shows that patients who receive naloxone may successfully use it on someone else to reverse an overdose. As of June 2019, New Mexico licensed providers are required to co-prescribe naloxone with opioid prescriptions of five days or more. The University of New Mexico Hospital (UNMH) has a Buprenorphine Induction Power Plan (BIPP) and an Opioid Withdrawal Power Plan (OWPP). Neither had an option for naloxone prescription upon discharge, and both power plans were underutilized resulting in missed opportunities for the highest quality care. Our aims were to add naloxone upon discharge to both the BIPP and OWPP and increase the usage of both power plans by at least 50% over three months.
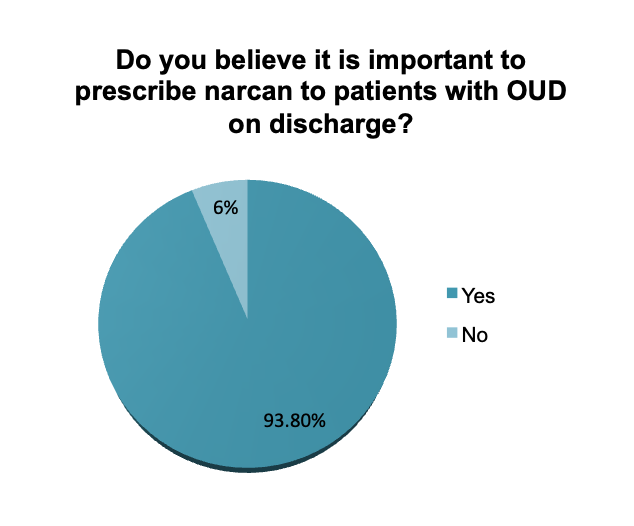
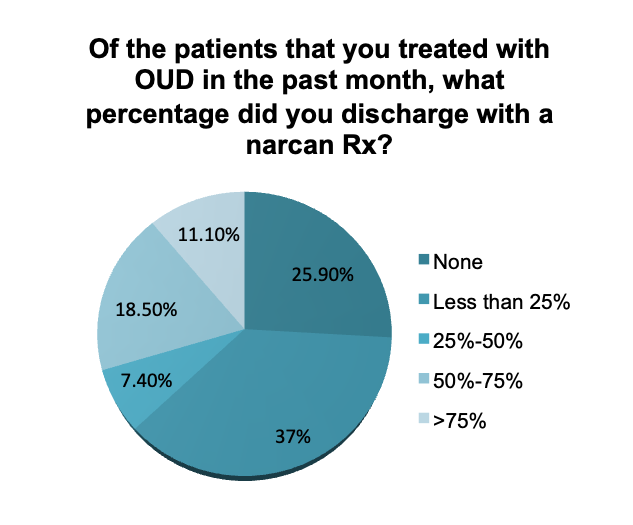
Methods: We administered REDCap surveys to UNMH providers to assess their knowledge of the OWPP and prescribing practices of naloxone to patients with OUD. No names or identifiable data were collected. A majority of respondents reported not using the OWPP because they did not know it existed. Additionally, From our provider survey we found a discrepancy between beliefs of importance of naloxone prescription and actual prescribing practices, as seen in the attached figures. Following Plan-Do-Study-Act Cycle 1, we identified that naloxone was not included in either the BIPP or OWPP. Informational sessions were held for family medicine, internal medicine, and advanced practice providers of various specialties to highlight the power plans as well as the recent addition of naloxone.
Results: Retrospective data obtained by the UNMH IT Department showed that pre-intervention OWPP usage was 15 times over 110 days, an average of 4.1 times/30 days. Post intervention OWPP usage was 58 times over 110 days, an average of 11.5 times/30 days, an increase of 180%.
Conclusions: Our student-led quality improvement (QI) project increases patient safety by increasing provider decisional support, efficiency of practice, and ease of prescribing Naloxone, helping providers comply with the new co-prescribing law. We hope to decrease the discrepancy between provider beliefs about the importance of naloxone and their prescribing rates. By adding naloxone to the power plans, this project connects inpatient management to outpatient pharmacy through the use of the electronic medical record (EMR), which has not been done at this institution, resulting in an interdisciplinary effort to manage Opioid Use Disorder (OUD) and remove barriers like transportation. We are hopeful that future data analysis will show an increase in the rate of naloxone prescription. Our research highlights the importance of ensuring providers are aware of existing power plans and that power plans meet the standard of care so they can be properly utilized. Our findings also demonstrate the power of QI initiatives to identify areas of improvement and effect change.