Background: Interhospital transfer (IHT) is a pathway by which many patients may receive procedures or specialty care not available at their local hospital. While IHTs present the opportunity for resource sharing between hospitals for the purpose of improved patient outcomes, the discontinuity of care and the acuity of the patients may adversely affect other quality metrics such as length-of-stay (LOS). This study aims to examine the indications and outcomes of patients accepted for IHT to better understand potential opportunities for improvement in the transfer process.
Methods: Our urban academic quaternary-care hospital is a member of a large multi-hospital health system. A retrospective chart review was conducted for all IHTs accepted from March 27th-June 30th 2023. Email communication sent by the accepting hospitalist was reviewed for information on the patient’s sending facility, the primary indication for transfer, and time period of acceptance. The electronic medical record was reviewed for outcomes including patient LOS, time elapsed from transfer acceptance to patient arrival, consulting specialties, mortality, and 30 day-readmission.
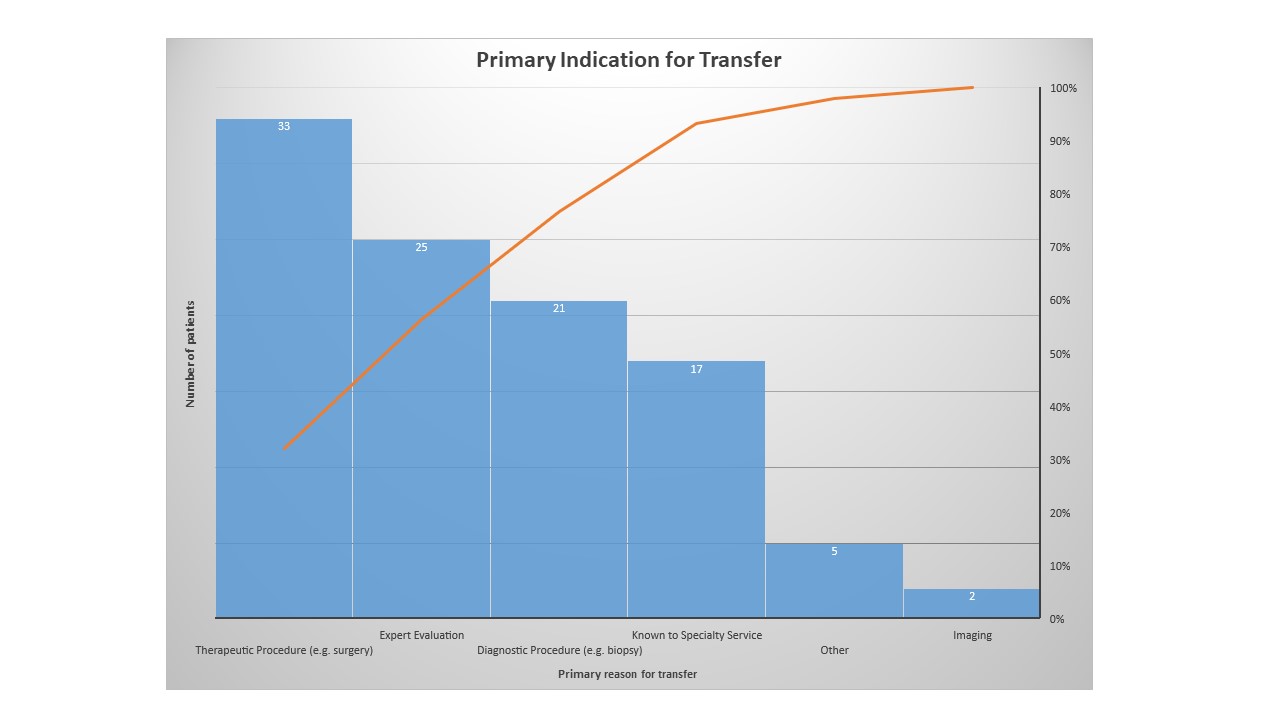
Results: There were 103 IHTs reviewed during the 3-month analysis period. Most transfers (68.9%) originated from one of six other hospitals within our health system, while 31.1% of patients were transferred from outside the health system. Of the IHTs, 71.1% had been seen in our health system within the last 2 years and most patients (68.9%) were accepted during the day. We found that 54 patients were transferred primarily for evaluation for a procedure, 25 for expert care from a specialty not available at the sending facility, 17 for continuity of care by a specialty service, 2 for diagnostic imaging, and 5 for other reasons such as family request. Of the patients transferred primarily for procedures, 33 were transferred for evaluation of therapeutic procedures such as thrombectomy or vascular stenting, while 21 patients were transferred for diagnostic procedures such as renal biopsies. Most patients (77.8%) received their intended procedure and on average, waited 2.5 days from time of transfer to procedure. The most commonly consulted specialty services were gastroenterology (19.4%), pulmonology (11.7%), and a multi-disciplinary pulmonary embolism response team (6.8%). Average LOS among transferred patients was 14.4 days at our hospital, compared to 8.8 days for all hospitalist patients in the same time period. Readmission rate was 22.3% in IHTs versus 14.5% in all hospitalist patients. Mortality was similarly higher in IHTs at 7.8% compared to 2.9% for all hospitalist patients.
Conclusions: While other studies have described handoff practices and safety outcomes for IHTs, few have described indications for transfers or services received. Our analysis demonstrated that the majority of patients were transferred for procedures or expert evaluation. While most patients received the intended procedure, 22.2% did not, indicating a potential improvement area for more rigorous screening for procedure candidacy prior to transfer. Additionally, the average 2.5 day time from transfer arrival until procedure date suggests opportunity to decrease LOS, such as a more detailed pre-operative evaluation at the sending site or coordinating procedure timing with patient arrival. Consistent with other studies, we found increased LOS, readmission, and mortality rates among IHTs.