Background: Accurate coding is paramount to hospital revenue generation and is often supported by a clinical documentation integrity (CDI) team made up of registered nurses and non-clinical coding personnel. Physician-led coding initiatives have demonstrated improvement in case-mix index and clinical documentation. We hypothesized that physician integration into CDI would result in a more robust improvement in accurate coding than CDI intervention alone. We report outcomes from integrating a physician-champion into our CDI education team with a comparison to prior attempts at coding and billing improvements in the same system by both our own CDI team and by a private coding education group.
Methods: A physician-leader within the department of hospital medicine learned the relevant American Medical Association Current Procedural Terminology (CPT) and CMS documentation guidelines and served as an advisor to both the CDI team and the physician team. Interventions included targeted education, the development of system-level EPIC dot phrases, bi-weekly coding tips, a hospitalist documentation algorithm, and a physician-supported educational lecture. Scorecards were developed and emailed to all participants monthly that contained group and personal average billing spread as compared with CMS average. Data collection was performed monthly by pulling relevant hospital codes from revenue. Codes retrieved included initial hospital codes for inpatient (99221-99223) and observation (99218-99220), subsequent codes for inpatient (99231-99233) and observation (99224-99226), critical care codes (99291-99292), and inpatient and observation discharge codes (99217, 99238, 99239). CPT code families were organized as initial inpatient, initial observation, subsequent inpatient, subsequent observation, and inpatient discharge codes. A weighted average was calculated for each possible CPT family and used to calculate the CMS average wRVU/encounter (assuming 1 CPT code per encounter). This data was used to determine a comparison between physician billing for each encounter type and CMS average (rather than just wRVU production) to allow for an accurate individual physician-to-CMS comparison. Accurate capture of CPT codes per encounter and elimination of duplicate charges was confirmed by using billing and revenue data rather than charging data.
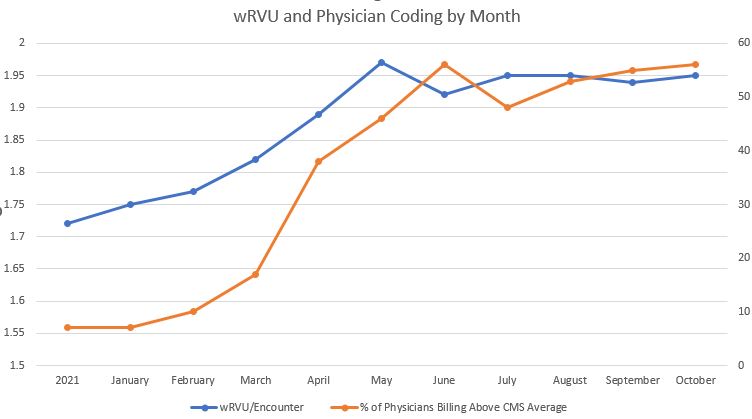
Results: Hiring a private company to perform CDI education resulted in a transient increase in wRVU/encounter from 1.6 to 1.8 over a 3-month period in 2017, but this rapidly returned to near 1.6 within 3 months of the intervention’s end. A pilot program to improve wRVU/encounter by targeting the lowest-performing hospitalists in 2018 resulted in transient increases in wRVU/encounter from 1.59 to 1.65, but was cut short due to the COVID-19 pandemic. Development of a physician-sponsored and CDI-nurse-lead educational plan resulted in a sustained, global improvement in wRVU/encounter from 1.75 to 1.95 within 4 months. This 11% improvement has been sustained over the following 6 months and is expected to increase as further targets of opportunity are realized. This change will result in over $1,500,000 in additional yearly revenue which was going unrealized.
Conclusions: Integration of an employed physician-advisor into CDI education demonstrated better overall improvement than CDI education alone or with hiring outside firms to support accurate coding. Consideration for dedicated physician-CDI support should be strongly considered.