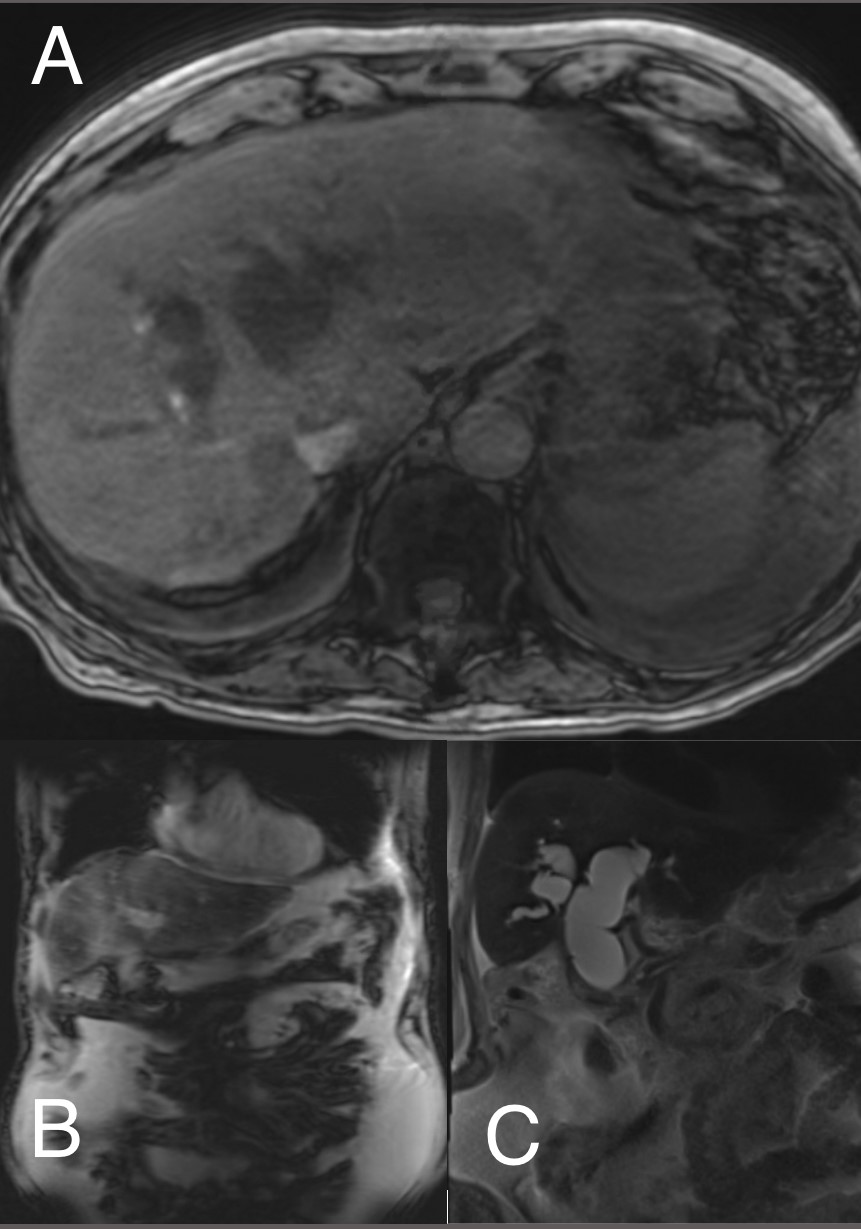
Case Presentation: We present a 96-year-old male who presented to the emergency department with syncope and worsening fatigue. He noted yellowing of his eyes and skin, clay colored stools and dark urine. He had a remote cholecystectomy but no prior liver disease and denied alcohol use.Physical exam revealed prominent jaundice and scleral icterus with a soft, nontender, but distended abdomen. Initial labs revealed significant hyperbilirubinemia with a total bilirubin of 18.4 mg/dL, direct bilirubin of 16.2 mg/dL, aspartate aminotransferase of 111 U/L and alanine aminotransferase of 88 U/L. International normalized ratio (INR) was 1.6 with a prothrombin time of 13.6 seconds. Computed tomography of the abdomen revealed a moderate to large amount of ascites with severe intra-and extrahepatic ductal dilation. Magnetic Resonance Cholangiopancreatography revealed severe intrahepatic and extrahepatic biliary ductal dilation with abrupt tapering of the common bile duct near the pancreatic head without an obstructing stone or mass. Signal characteristics of the liver and pancreas were suggestive of primary hemochromatosis and cirrhosis. Iron studies were ordered and revealed an iron level of 149 ug/dL, iron percent saturation of 114, and a ferritin of 2,157 ng/mL The paracentesis revealed a serum ascites albumin gradient score of 3.2 and ascitic protein of 1.6 g/dL, supporting portal hypertension and cirrhosis. Unfortunately, the patient’s liver function continued to worsen. Gastroenterology recommended against aggressive treatment or pursuing genetic testing, as the patient had imaging and iron studies supporting the diagnosis. He was discharged with home hospice and the diagnosis of new onset cirrhosis with acute liver failure secondary to primary hemochromatosis.
Discussion: Hereditary hemochromatosis (HH) is a primarily autosomal recessive disorder of iron overload. Once thought to be a rare diagnosis, today, it is one of the more common genetic diseases in the United States. Untreated, patients can experience early death with common etiologies including heart failure, cirrhosis, diabetes, and hepatocellular carcinoma. Presenting symptoms include fatigue, joint pain, skin pigmentation, new onset diabetes, and impotence. Initial Work-up includes liver function tests, serum ferritin, and iron studies. Elevations in serum iron, ferritin levels greater than 300ng/mL in men and 200ng/mL in women, and transferrin saturation greater than 45 percent in men and 55 percent in women support a diagnosis of hemochromatosis. Magnetic resonance imaging remains the most sensitive and specific imaging. Testing for two common HFE gene mutations, C282Y and H63D, is appropriate in individuals with evidence of iron overload. Lastly, testing is appropriate for first-degree relatives of an individual diagnosed with HH.
Conclusions: With most patients presenting in the 4th -6th decades of life, we presented a unique patient that defied the odds and survived 96 years prior to the onset of acute liver failure from primary HH. Upon literature review, it is exceedingly rare to be diagnosed in the 10th decade without prior symptomatology, especially presenting as acute liver failure. Hemochromatosis can present with an array of symptoms and complications. With this case, we hope to encourage clinicians to keep hemochromatosis on their differential diagnosis for acute liver failure, even if the patient is a 96-year-old without a significant history of liver disease.