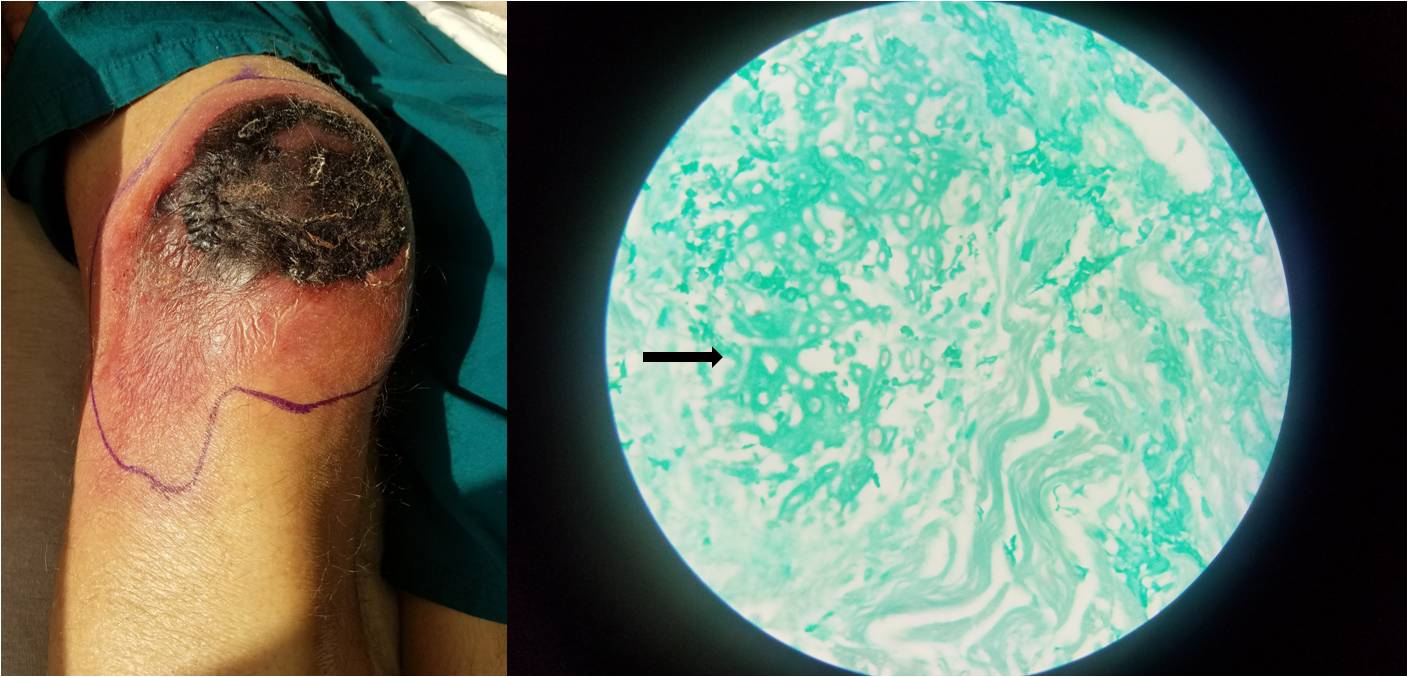
Case Presentation: A 57-year old man with a history of chronic lymphocytic leukemia, complicated by treatment-related myelodysplastic syndrome (MDS), presented with a large, painful, dry ulcer with black eschar on his right knee. He was afebrile and hemodynamically stable, but in moderate distress due to the pain and swelling of his right knee. Initial lab studies demonstrated pancytopenia with a serum WBC count of 500/μL. Although knee aspiration did not show evidence of septic arthritis, a punch biopsy revealed abundant mucormycosis as the culprit organism in the gangrenous wound. Multiple blood transfusions and broad spectrum antibiotics including antifungals were initiated, and a collaborative discussion took place between medicine and surgical services regarding wound management. Although surgical debridement or amputation was recommended as the definitive cure, both were deemed extremely high-risk and ultimately not offered given his poor healing potential and his baseline prognosis of 6-12 months. The decision was therefore made to treat the patient palliatively in hospice with liposomal amphotericin B and posaconazole despite the risk of cumulative nephrotoxicity.
Discussion: This case demonstrates the unique challenge of managing cutaneous mucormycosis (CM) in patients with severe pancytopenia. CM can be either superficial or gangrenous – the latter of which is more common in immunocompromised patients. Penetrating trauma remains the major cause of primary cutaneous infection with mucormycosis, and even very slight insults to skin integrity have been attributed. Treatment is typically aggressive, with extensive local surgical debridement and the use of high-dose amphotericin B. Surgical interventions have been shown to significantly improve local disease control, as the angioinvasive nature of mucormycosis can lead to thrombosis, decreased tissue blood supply and healing, and inhibited penetration of antifungal medications. Primary CM carries a reported overall mortality rate of 29.4% in cases of dissemination, and is especially fatal in those with neutropenia (60%) or no surgical intervention (73%). Multiple factors must be considered regarding the appropriateness of aggressive surgical intervention in severely neutropenic patients, including post-operative wound healing potential, background prognosis, renal function (given amphotericin B toxicity), and the patient’s own goals of care.
Conclusions: Patients with neutropenia are at an increased risk for primary CM, which can be severe and fatal. However, decreased wound healing potential in these patients complicates the decision to pursue aggressive, surgical treatment. Multiple factors should be considered in determining the best course for the individual patient.