Background: One of the Society of Hospital Medicine (SHM) core competencies (listed as Principle 7) is that Hospitalists provide effective clinical resource utilization. Examples: cost effective care, high-value care, and designing processes that address cost per stay and readmissions. Optimized inpatient throughput has been shown as a strategy to improve overall hospital flow, including streamlined ED admissions to Hospitalist floors. Patient satisfaction decreases when emergency department (ED) length of stay (LOS) exceeds two hours.
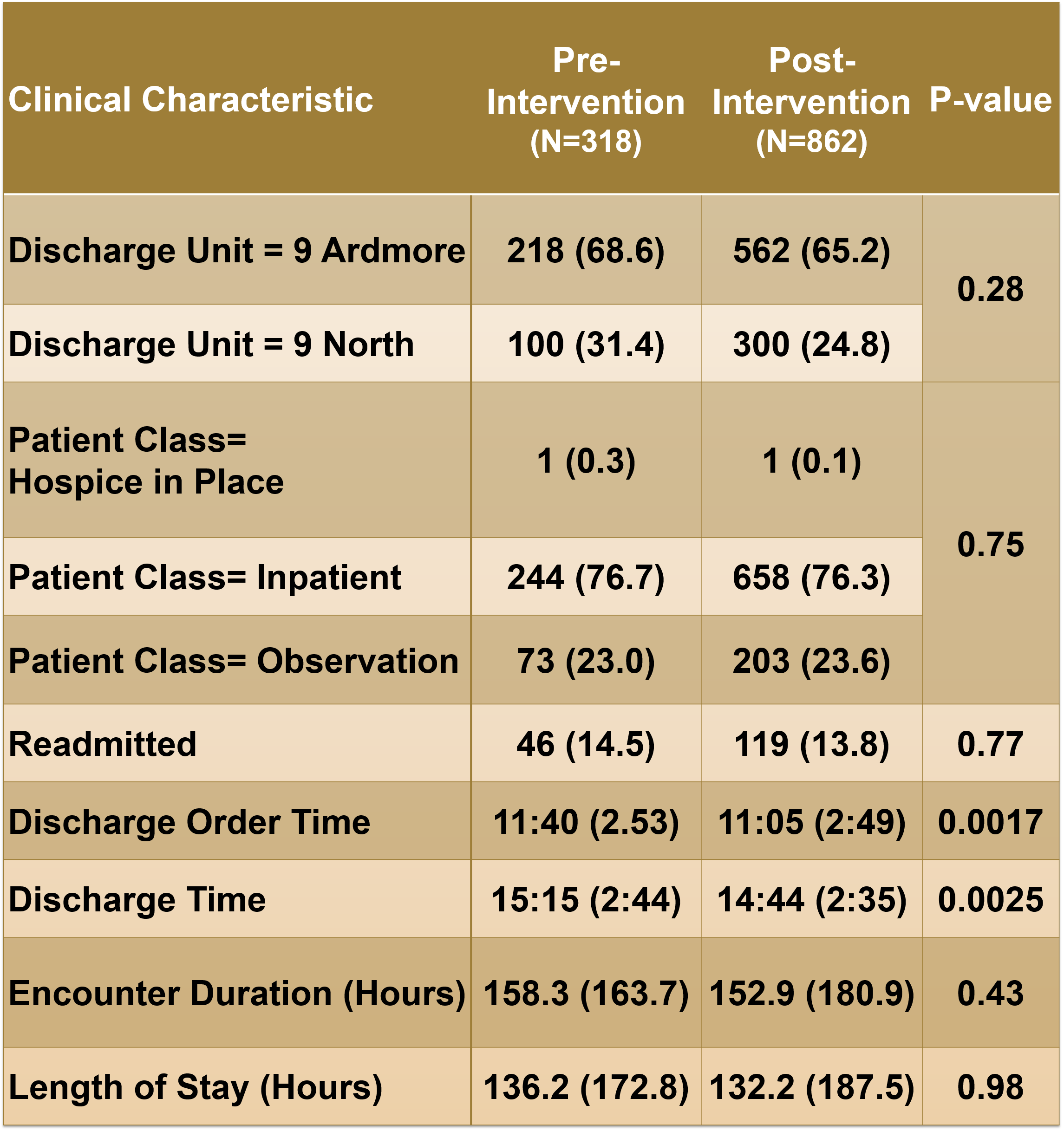
Methods: Lightening Huddle was introduced in November 2017 to provide a streamlined process for conducting discussions about plan of care and discharge. We performed SWOT analysis (Strengths, Weakness, Opportunities and Threat) involving all the key stakeholders on Hospitalist Units, including Physicians, Advance Practice Providers, Nursing, Care Coordination, Pharmacy, Administration and Care Navigation teams. We determined following major elements that were crucial for discharge planning: 1) Patient demographics (room number and name), 2) discharge status, 3) discharge disposition, 4) ability to transfer to discharge lounge or holding unit 5) barriers to discharge. By using a magnetic white board divided into five columns (Discharge status/ Disposition/ Safety to go to 5C/ Discharge Lounge/ Barriers) and a defined script, we aimed to limit the morning huddle to less than 10min for 38 bed unit, yet covering the important aspects of discharge planning. We compared pre- and post-intervention categorical outcomes with chi square tests and continuous outcomes with t-tests.
Results: The Lightning Huddle resulted in reduced morning huddle time compared to prior to intervention (mean 8.29 minutes, standard deviation 2.15 minutes). This resulted in significantly earlier discharge order time (provider placing discharge order) (p=0.0017) and discharge times (patients leaving from the unit) (p=0.0025). The Lightning Huddle was associated with shorter encounter duration (p=0.43) and length of stay (p=0.98), but these differences were not statistically significant. During the study (November 2017 to February 2018), through efficiency of communication in Lightning Huddle, a cumulative of 18.5 patient days were saved.
Conclusions: Lightning Huddle was crucial in limiting the morning huddle time and streamlining the process of interdisciplinary team discussion, thereby providing more time for the providers and staff to tend to their patients and other clinical responsibilities. Lightning Huddle improved patient flow (throughput) and provided an effective method of bed capacity management. A future randomized study might improve upon demonstrating the benefits of the Lightning Huddle procedure for reducing encounter duration and length of stay.