Background: High need patients are characterized by medical complexity, high amounts of health acute care utilization and disproportionate costs[1]. Recent studies have characterized worsening of loneliness in the general population, however, it has not been characterized in the high need population. We hypothesized that increases in loneliness would be associated with increasing symptoms of depression; increasing alcohol use, and increasing inpatient admissions.
Methods: We performed a cross sectional study of a high need cohort enrolled from a hospital medicine based comprehensive care program at a tertiary care academic hospital. We enrolled participants between July of 2022 and August of 2023. We included adults (18 or older) with multimorbidity (Charlson Score[2] >3), or high risk for readmission (Defined by LACE readmission risk score[3] >30). All participants provided informed consent. We measured loneliness among participants using the validated De Jong Giervald Loneliness Scale[4]. We stratified patients into not lonely (Score 0-2), moderately lonely (3-8), and severely lonely (>8). We measured depression symptom burden with the PHQ9[5], a validated instrument with scores ranging from 0 (no symptoms) to 27 (high symptom burden). We assessed alcohol use using the Alcohol Use Disorders Identification Test AUDIT-C[6], with scores ranging from 0-12. We additionally measured the number of inpatient admissions in the year prior to enrollment. To test our hypotheses, we performed proportional odds logistic regression analysis, with the loneliness score as the independent predictor, and each of the outcome variables, as continuous outcomes. All models were adjusted for age, gender, race (white vs non-white), and LACE score.
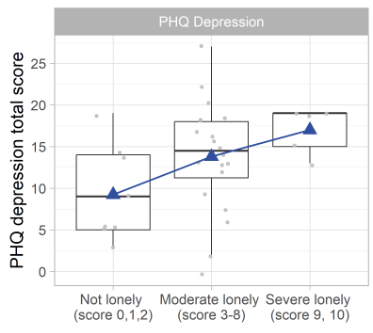
Results: We enrolled 34 patients during the study period. 53% of patients were female (n=18), 35% of patients were Black/African American race (n=12), with a median Charlson Comorbidity Score of 5.0 (IQR 4.0 to 6.8), and a Median LACE readmission risk score of 74.5 (60.0 to 79.8). Nine (26%) of the patients were not lonely at baseline, 20 (59%) patients were moderately lonely, and 5 (15%) patients were severely lonely. Median PHQ9 depression scores were 14.0 (IQR 9.0 to 18.0), AUDIT-C scores were 0.0 (IQR 0 to 1.0), and number of inpatient admissions in the year prior was 2.0 (IQR 1.0 to 2.8). In multivariable analysis, an increasing loneliness score had a 2.39 (95% CI 1.16 to 4.95) increased odds of having a greater PHQ total score. Figure 1 displays Box Plots of PHQ9 score by loneliness category, visually demonstrating this positive relationship. Loneliness scores were not associated with alcohol use (OR = 1.18, 95% CI 0.55 to 2.53) or number of inpatient admissions (OR = 0.78, 95% CI 0.43 to 1.43).
Conclusions: Loneliness is of increasing concern, given recent reports of associations with cognitive decline, poor mental health, and mortality[7]. We demonstrated that loneliness is highly prevalent in the high need population commonly cared for by hospitalists, with 74% of patients experiencing moderate or severe loneliness. Similar to the general population, loneliness is strongly associated with depression; however, it was not associated with alcohol use or hospital utilization in the past year after adjusting for traditional readmission risk. Findings should be confirmed in larger cohorts of high need populations. Interventions are needed to better identify and address loneliness in this high-risk population.