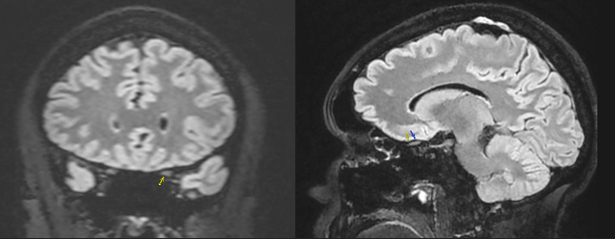
Case Presentation: A 44-year-old man with no significant medical history was referred from our ophthalmology clinic with clinical concern for optic neuritis. One week earlier, he noted acute onset of left eye discomfort and blurred vision which evolved to central vision loss and brightness desaturation, accompanied by new headaches. Initial exam and lab work were otherwise unremarkable other than a mild elevation of C-reactive protein to 5.58 (< 5.1 mg/L). Contrast-enhanced brain and orbital magnetic resonance imaging (MRI) identified left optic perineuritis involving the distal intra-orbital, intra-canalicular and pre-chiasmatic portions of the optic nerve (Figure 1). On empiric high-dose systemic steroids, he endorsed improvement of ocular symptoms and headache. He also disclosed an improvement in intermittent dyspnea and cough which had been present for 6 months. Further evaluation with non-contrast CT chest imaging showed bilateral, peribronchovascular pulmonary micronodules with hilar and mediastinal lymphadenopathy. Additional work up revealed a normal serum angiotensin converting enzyme (ACE) level, negative autoimmune serologic testing, and vitamin D deficiency. A bronchoscopy with biopsy found non-necrotizing granulomas with negative AFB stains and microbial growth. Six months following the diagnosis of systemic sarcoidosis, the patient continues to endorse clinical improvement while undergoing a prolonged steroid taper.
Discussion: Optic perineuritis (OPN) is an uncommon form of orbital inflammatory disease, characterized by optic nerve sheath inflammation resulting in varying degrees of optic nerve dysfunction (1). The clinical presentation may mimic optic neuritis. The majority of patients present with acute visual loss, eye pain, or both. Visual blurring, dimming, and “spots” in vision are often described. Pain with eye movement is typically more severe or persistent than in optic neuritis. The mean age of presentation is between 40 and 60, with a potentially higher incidence in women (1,2). Diagnosis is typically based on a combination of clinical and contrast-enhanced orbital MRI findings (3). Rarely, an optic nerve biopsy is necessary. Most cases are idiopathic but as in our patient, OPN can be a manifestation of systemic disorders including sarcoidosis, IgG4-related disease, inflammatory vasculitides, IBD, syphilis, tuberculosis, HSV, leukemia, and primary or metastatic malignancies. In the absence of an obvious underlying cause for OPN, systemic work-up should be performed with a lumbar puncture and testing for syphilis, ACE level, ANCA, and IgG4. OPN typically has a relatively good prognosis. There is no known association between development of OPN and multiple sclerosis. Corticosteroids with a slow taper remain the mainstay of therapy (4).
Conclusions: Optic perineuritis is an uncommon inflammatory disease of the optic nerve sheath which can be primary or secondary in etiology. We describe a case of undiagnosed systemic sarcoidosis masquerading as optic neuritis and highlight the importance of further investigation beyond the clinical impression since early identification and treatment of potential conditions associated with optic perineuritis is crucial for optimal patient outcomes.