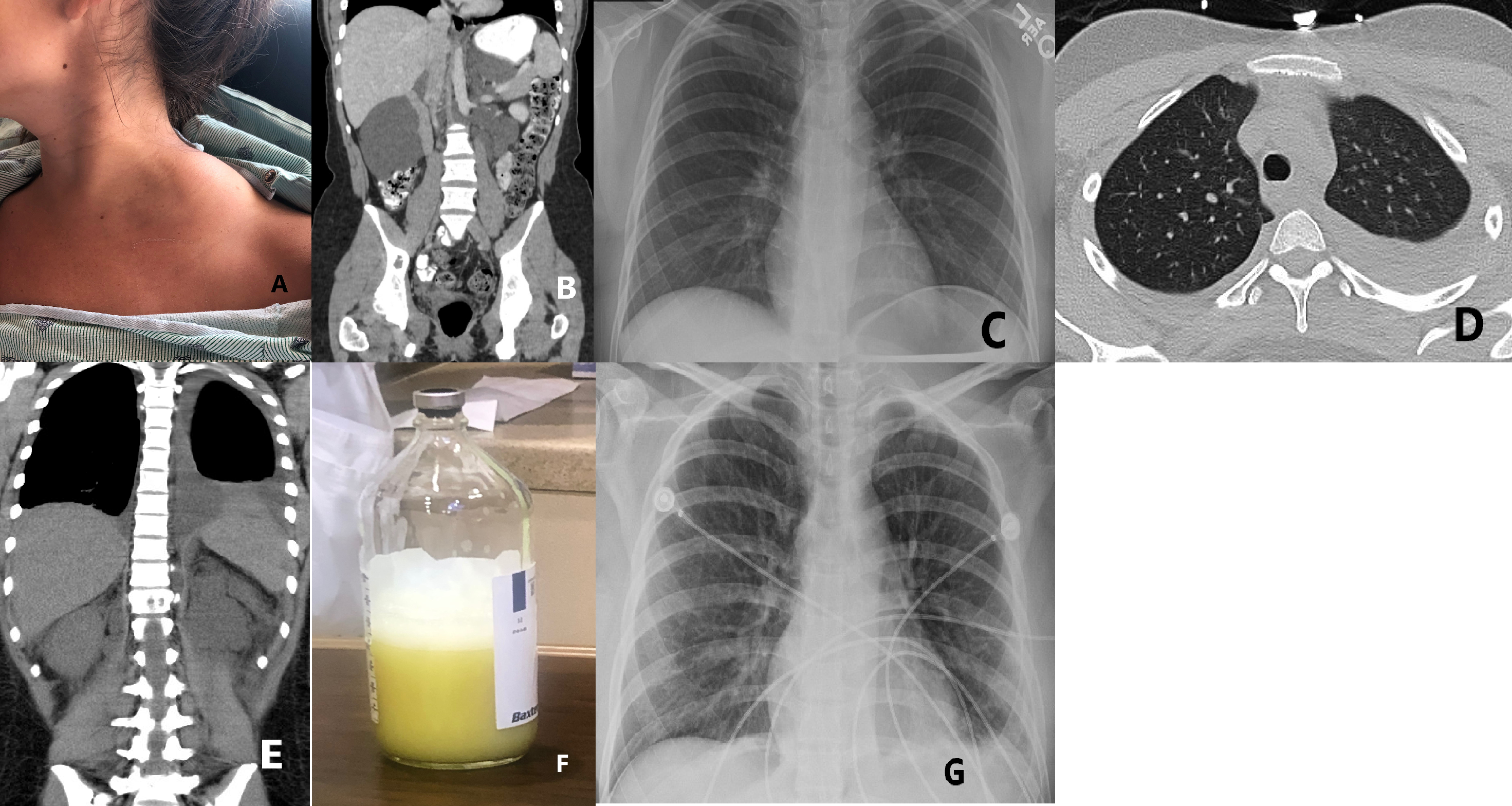
Case Presentation: A 26-year-old female with lymphangiomatosis presented to the emergency department with fever and malaise of one day duration. She denied headache, cough, nausea, dysuria, or rash. Vitals were notable for elevated heart and respiratory rate. Initial lab work revealed a WBC of 5.9 with a neutrophilic predominance of 99%. This neutrophilia led to further investigation with a CD4 count, which was notably decreased at 29. Sepsis protocol was initiated with aggressive volume resuscitation and empiric antibiotics. Blood cultures grew Group B Streptococcus sensitive to IV ceftriaxone. Imaging studies done at admission reaffirmed a history of stable lymphangiomas in the left hemithorax and bilateral retroperitoneum, without pleural effusion (Image A, B, C). On the second day of admission, following large volume fluid resuscitation, the patient was increasingly tachypneic and required increased oxygen supplementation. CT chest discovered new bilateral pleural effusions left greater than right (Image D, E). A diagnostic and therapeutic thoracentesis was performed which removed 500 cc of cloudy yellow fluid (Image F). Pleural fluid studies were remarkable for a triglyceride level of 335 mg/dL, an LDH of 264 U/L, and a protein level of 3.2 g/dL, consistent with chylothorax.Prior management of the patient’s lymphangiomatosis included propranolol, a well-documented treatment option for the prevention of lymphatic malformations [1,2]. However, this had been discontinued prior to admission due to lack of clinical response. On discharge, a chest X-ray showed no reaccumulation of chylothorax (Image G) and the patient was started on subcutaneous octreotide, prednisone, and a low-fat diet to prevent future recurrence. Cardiothoracic surgery recommended medical management over thoracic duct ligation as this was the patient’s first chylothorax.
Discussion: Lymphangiomatosis is an uncommon disorder of lymphatic development, thought to be caused by an in-utero malformation leading to persistent dilation of lymphatic vessels between 14 and 20 weeks of gestation [3]. The disease manifests in a myriad of ways but is characterized by benign lymphatic tumors that may compress surrounding structures.
Conclusions: This case represents a rare consequence of chylothorax in the context of lymphangiomatosis, and more specifically a temporal association with large volume resuscitation as necessitated by sepsis secondary to bacteremia. There have been case reports linking chylothorax and lymphangiomatosis, but usually as the presenting finding [4,5]. The temporal association, and presumed causal link, between fluid resuscitation and development of chylothorax in a patient with lymphangiomatosis has not been established. This case may serve to better inform the risks associated with volume overload in patients with lymphangiomatosis, or with other disorders of lymphatic drainage.