Background: Growth faltering or failure to thrive is a common cause of admission in infancy and early childhood. In the United States, approximately 2-10% of children experience lower-than-expected growth associated with malnutrition (Tang et al). Growth faltering accounts for 3-5% of pediatric hospitalizations (Mazze et al, 2019). Malnutrition is associated with complications of increased risk for infection, developmental delay, and long-term consequences such as increased rates of metabolic syndrome and cardiovascular disease (Grey et al). Poor growth is commonly due to inadequate nutritional intake, which can be associated with feeding difficulty and behavioral factors as well as social determinants of health such as food insecurity (Tang et al, 2021). We identified the areas most affected by admissions for malnutrition across the catchment area for a major pediatric academic hospital as part of an ongoing quality improvement effort to reduce need for hospital admission.
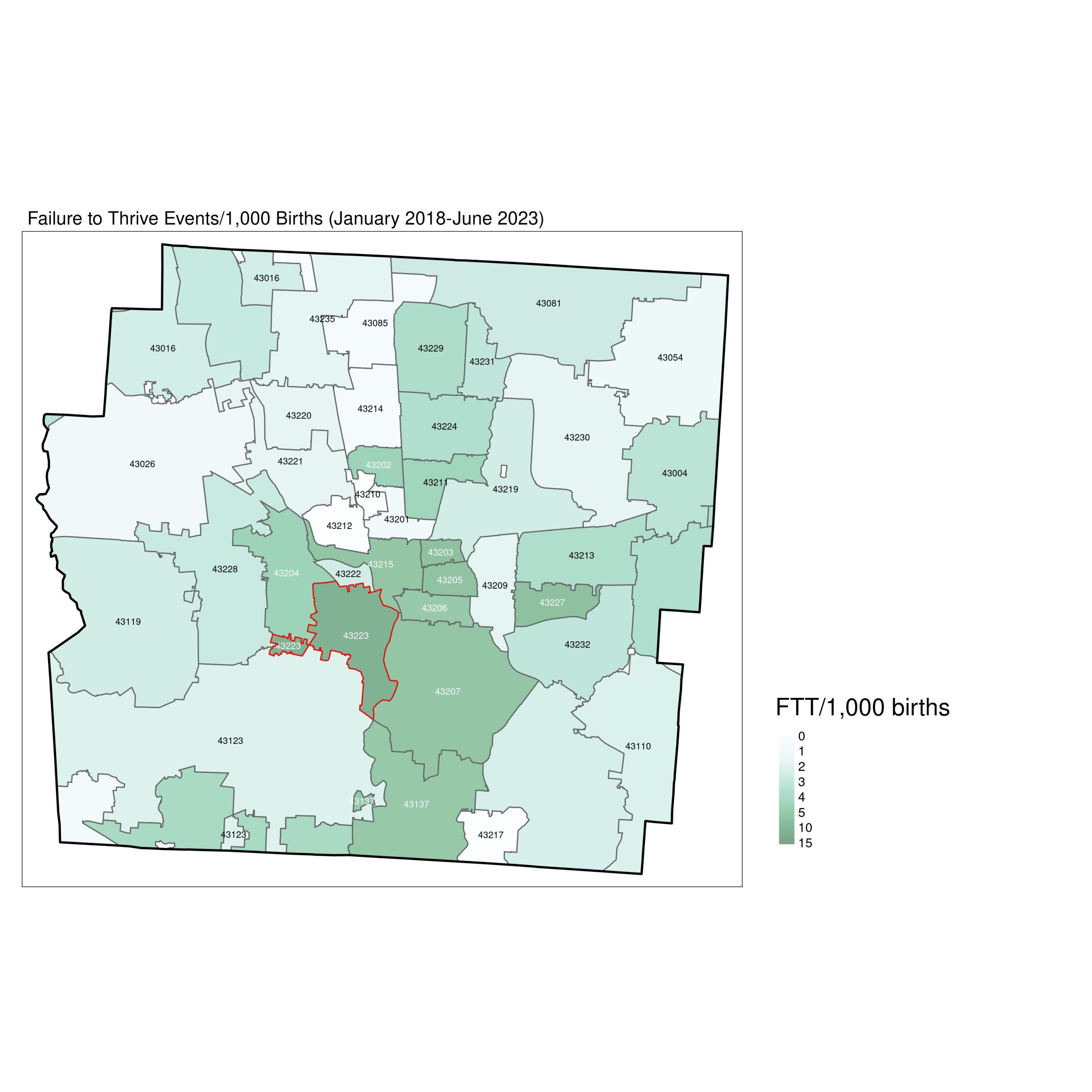
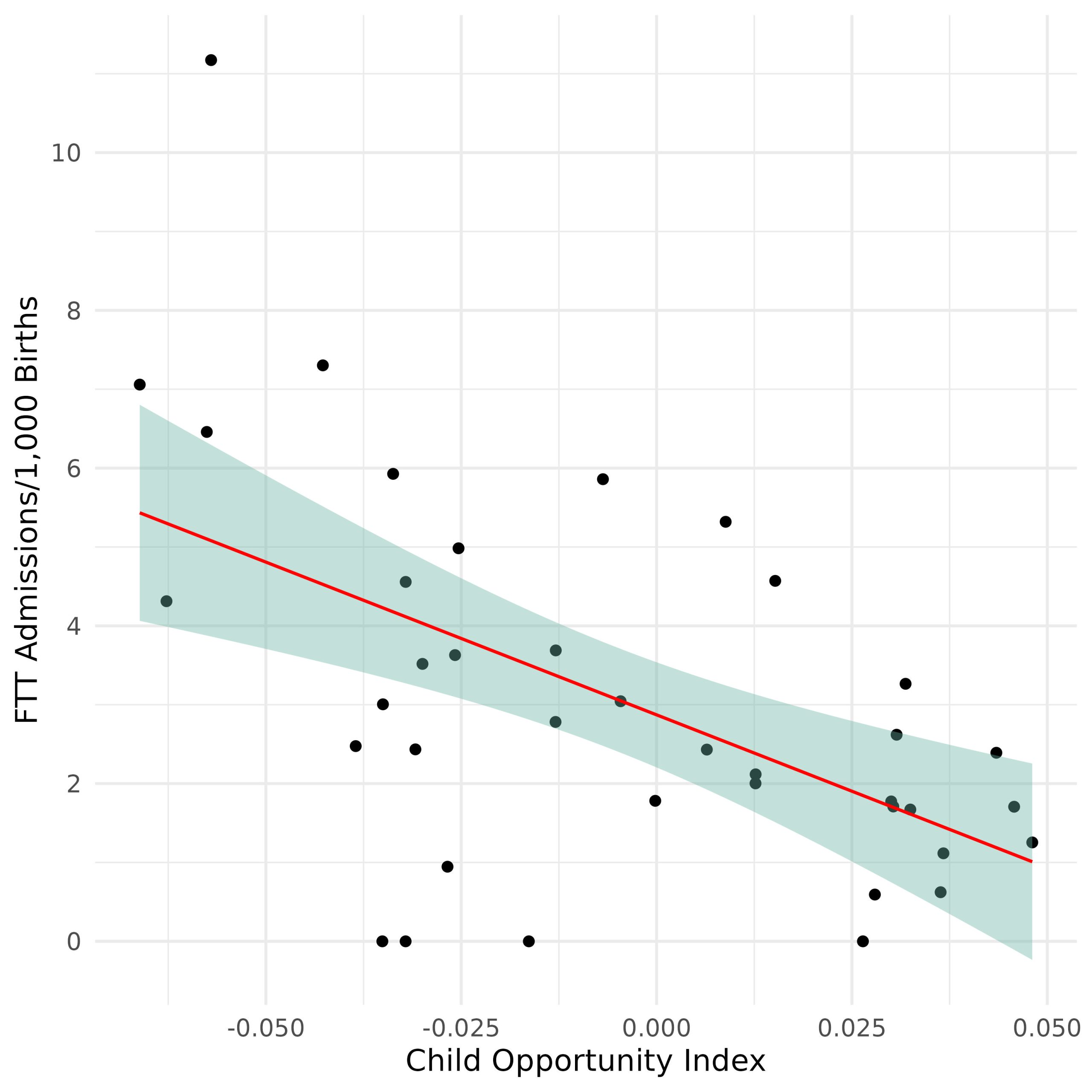
Methods: Our patient population included all children aged 0-5 years admitted for failure to thrive (ICD R62.51) from January 2018-June 2020. Birth counts by ZIP code from the Ohio Department of Health were used to calculate the FTT event rate per 1,000 births in each ZIP code during the study period. Statistical analyses were limited to Franklin County as a conservative estimate of our hospital’s catchment area for FTT admissions. The Kulldorf Spatial Scan Statistic (1997) allowed us to identify areas with disproportionately high rates of admissions, controlling for the number of births. Pearson’s correlation coefficient was calculated to test for a relationship between FTT admission rates and area-level opportunity, as measured by the Child Opportunity Index 2.0 (Acevedo, Clemens 2020). All data analyses were conducted in R version 4.2.2 (R Core Team) with the tidyverse family of libraries (Wickham, et al 2019) and the SpatialEpi package (Kim, Wakefield, Moise, 2023).
Results: We found a disproportionately high number of admissions for early childhood malnutrition in one southwest ZIP code near downtown Columbus with an FTT rate of 11.2/1,000 births (figure 1). In Franklin County, the FTT admission rate was significantly, negatively correlated with the COI (ρ=-0.547, p< 0.001), (figure 2).
Conclusions: The incidence of admission for childhood malnutrition resulting in growth faltering or failure to thrive is not equally distributed in the population of Central Ohio. This study demonstrates a higher event rate of admissions than expected in ZIP codes with worse social determinants of health conditions as measured by the Childhood Opportunity Index. This correlation suggests that areas with less opportunity have greater admissions for failure to thrive or growth faltering. The results of this analysis provide a basis for further investigation into the specific antecedents that drive malnutrition and feeding difficulty in these communities resulting in hospital admission. We have started further inquiry into these antecedents in an upcoming qualitative review and needs assessment with local providers and community members to identify areas for intervention to reduce admissions and the excessive burden of early childhood malnutrition.