Background: Provider engagement is a key component of improving healthcare delivery in any healthcare setting. Characteristics of burnout are prevalent among healthcare providers and have been associated with lower engagement, increased errors and poor long term sustainability in the medical profession. In the era of increased quality, safety, experience and value measures, demands on providers are increasing, but few healthcare systems are deliberately focusing on the provider experience of work as a critical step to improving providers’ capacity to engage in key organizational priorities for improvement.
Purpose: This intervention describes an approach for healthcare systems to measure the provider experience of work and to improve that work experience.
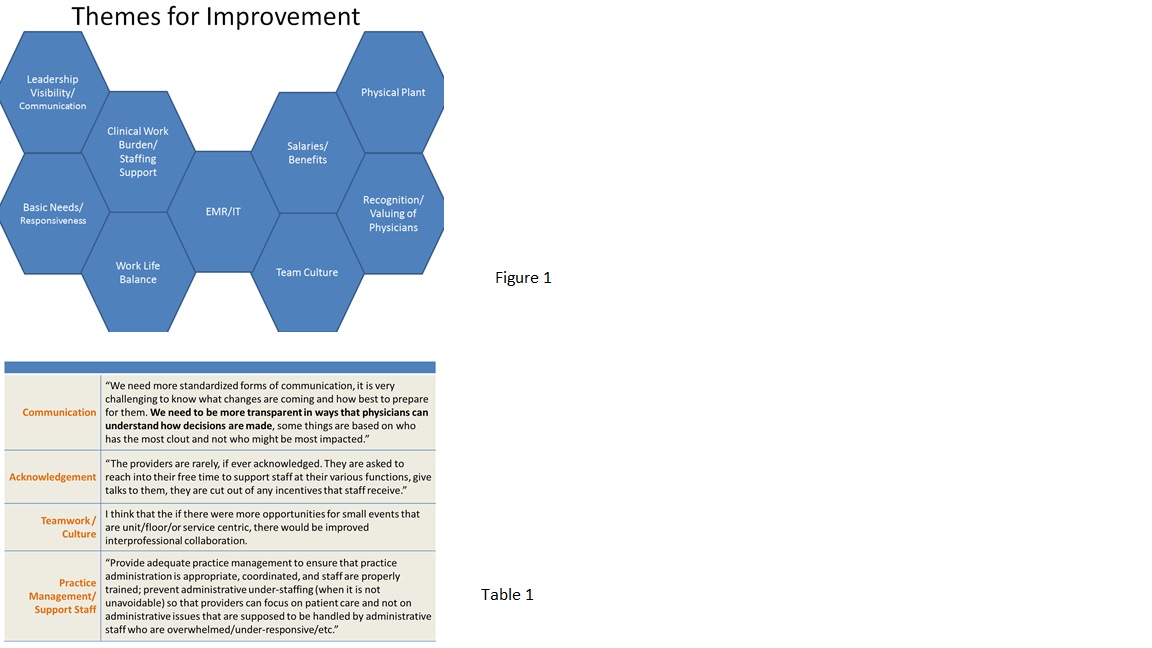
Description: In 2014, we sought to measure the experience of work of 1619 attending physicians across all clinical departments at our academic, urban medical center. Using a Net Promoter Score survey question methodology and online survey tool, we asked attending level physicians to quantitatively rate their likelihood of recommending our organization as a place to work and come for care as well as to describe their comments for improvement. The overall quantitative result for “place to work” was negative 11 ( (scale -100 to +100, response rate 42%), where high performing organizations score higher than positive 50. Analysis of the comments (Table 2) led to 9 themes of problem areas (Figure 1) which were broadly shared and explored further through public forum town halls, focus groups and individual interviews conducted by our Medical Director of Patient and Provider Experience and Chief Medical Officer. Follow up included raising awareness of problem areas with all levels of leadership and intervening on both “low hanging fruit” (ie. keeping call rooms updated and clean or including providers in the staff incentive program) and high priority items (ie. elbow to elbow coaching and optimization of EMR workflows for providers). A web site was created to share progress on improvements and to solicit input from physicians on further improvement ideas. High performing departments shared their stories stimulating further activities among other departments, while several units used mini versions of the same survey to look for ways to improve the work experience specifically in their own units or clinics.
Conclusions: Asking providers to rate their experience of work in an academic medical center provided an easy and efficient baseline measure of performance and a clearer understanding of the major barriers providers face working in our health system. The baseline quantitative measure will be used to compare annual follow up results. The themes generated from qualitative data provided concrete, actionable information and allowed further engagement of providers to generate solutions. The survey and its follow up functioned to let providers know that health system leadership values these problems and is responsive.