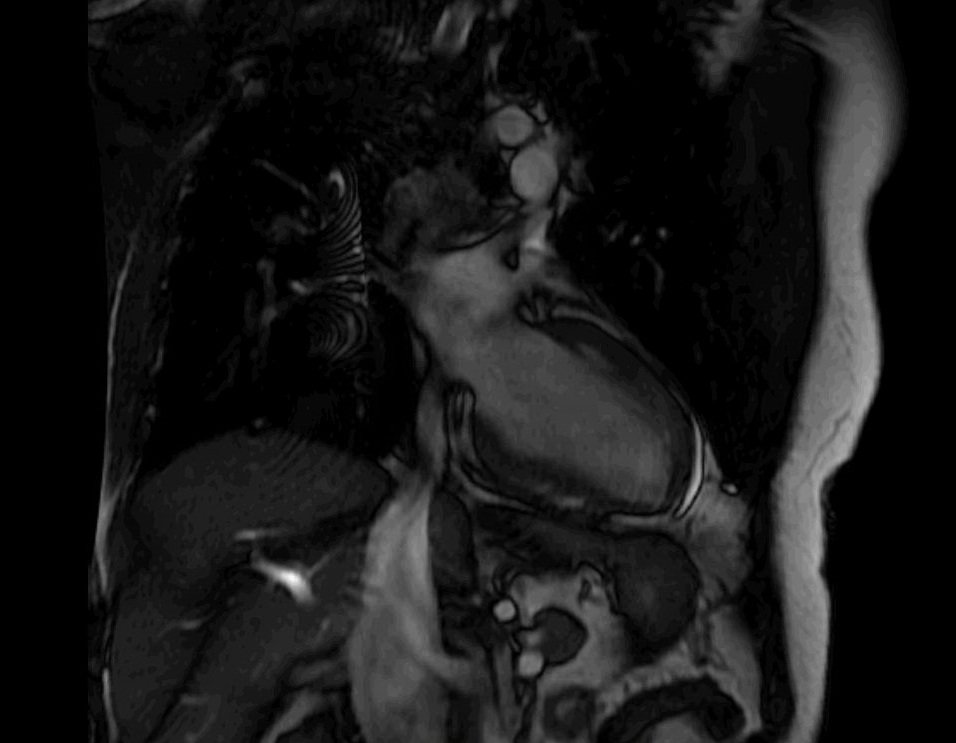
Case Presentation: A 45 year old African American male with sarcoidosis (2009 lung biopsy) was brought by EMS after an out of hospital ventricular fibrillation cardiac arrest. With ACLS, ROSC was attained after 20minutes. He had no family history of sudden death or heart disease. He did not engage in any toxic habits. Exam showed tachycardia but regular rhythm without additional heart sounds or murmurs, rhonchorous breath sounds, and subcutaneous nodules along his lower extremities. Labs were notable for a peak troponin of 0.95ng/mL, but urine toxicology, alcohol level, electrolytes, BNP, TSH, HgA1c and lipid panel were normal. EKG showed sinus tachycardia but no ST segment changes. Cardiac catheterization showed non-obstructive coronary artery disease. Echocardiogram (TTE) revealed a left ventricular ejection fraction (LVEF) of 35%. Cardiac MRI became indicated. It showed transmural late gadolinium enhancement in mid to apical anteroseptal, inferolateral and lateral walls, as well as subendocardial enhancement in the basal anterolateral walls. The patient was initiated on prednisone 40mg daily and received an implantable cardioverter-defibrillator (ICD).
Discussion: In the U.S. cardiac sarcoid occurs in up to 28% of patients with sarcoidosis. Although our patient had known pulmonary sarcoid, involvement of lungs is not predictive, nor does it correlate with cardiac sarcoid severity. Endomyocardial biopsy was obviated given its low sensitivity, but the certainty of cardiac sarcoid underlying the patient’s cardiac arrest was substantiated by fulfillment of diagnostic criteria established by The Heart Rhythm Society. He had an extra-cardiac affirmed sarcoid diagnosis via lung biopsy and met >1 clinical criterion by exclusion of obstructive coronary artery disease, TTE revealing a LVEF <40% and late gadolinium enhancement on cardiac MRI. Optimal management for cardiac sarcoid remained controversial. Aside from warranting an ICD as secondary prevention, the utility of corticosteroids (CS) remains dubious. The American College of Cardiology expert opinion suggests 30-40mg prednisone daily, reassessment after 1-3months and tapering over 9-12months. The patient was placed on this regimen despite there being no randomized, controlled trials or prospective comparisons on CS dosing to certify a benefit. A Japanese study, however, elucidated that CS led to 5 year survival rates in 75% of patients treated and up to 89% in those treated with LVEF >50%. Our patient had a reduced LVEF, but with ICD and CS, his chance of recovery was optimized.
Conclusions: While pulmonary involvement is the most common manifestation of sarcoidosis, one cannot overlook the gravity of cardiac involvement. Management recommendations for cardiac sarcoid are limited and largely governed by expert opinion and retrospective analyses. We hope our case will raise awareness for cardiac sarcoid to promote advancements in pinpointing optimal CS dosage and course, as well as extend efforts to establish reliable screening and prevention.