Case Presentation: A 33 year-old female presented to an outside facility with a few days of gradual onset abdominal pain with nausea and vomiting. On presentation, vital signs were notable for tachycardia. Examination showed periumbilical tenderness without rigidity or guarding. Labs were remarkable for leukocytosis and normocytic anemia but normal lipase. CT of the abdomen and pelvis showed small bowel wall thickening with minimal ground-glass changes in the mesentery suggestive of enteritis.
Her symptoms did not improve despite conservative treatment, so she underwent an EGD and colonoscopy were unremarkable. However, she was treated with ciprofloxacin and metronidazole and discharged home after some improvement in her symptoms.
She presented again a few days later at our facility with recurrence of her abdominal pain, nausea and vomiting. An EGD with enteroscopy that showed a jejunal bezoar resulting in near total small bowel obstruction. A push enteroscopy showed multiple, non-bleeding, gastric and jejunal ulcers. She was started on steroids with attempt to reduced small bowel wall inflammation to help passage of the bezoar.
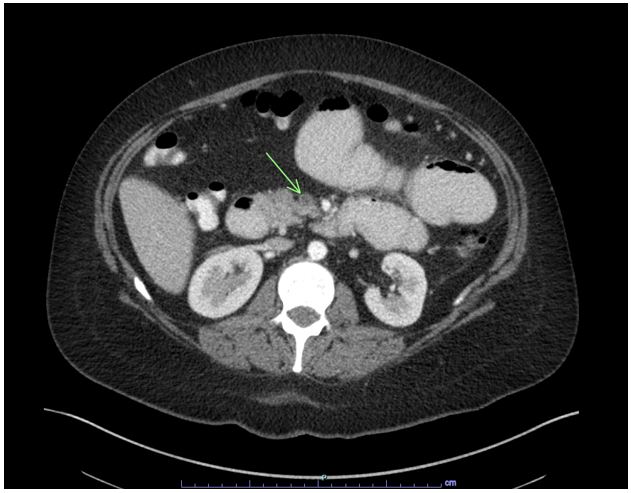
Her outside hospital CT scan was requested and upon review by our radiologists, a superior mesenteric vein thrombus was seen. A repeat CT abdomen showed dilation of the duodenum and jejunal loops proximal to the known foreign body and signs of intestinal ischemia and bowel perforation around the loop of ileum. An exploratory laparotomy that revealed small bowel perforation adjacent to the bezoar necessitating partial small bowel resection. Her symptoms improved, and she was discharged home and with follow-up for evaluation of a hypercoagulable state.
Discussion: Mesenteric venous thrombosis (MVT) is an uncommon cause of mesenteric ischemia. MVT usually involves the superior mesenteric vein (SMV) and rarely involves the inferior mesenteric or portal veins. The diagnostic modality of choice is CT angiography which reveals venous filling defects in mesenteric veins during the venous phase. The resultant venous occlusion is sufficient to produce ischemia. Our patient most likely developed the subacute form of SMV thrombosis which led to bowel wall edema and ischemia resulting in bezoar formation, small bowl obstruction, and untimely perforation.
Once the diagnosis is made, it is important to look for predisposing factors such as local intra-abdominal inflammatory processes as well as prothrombotic states such as malignancies or myeloproliferative disorders. Management of MVT is aimed at preventing bowel infarction and recurrent thrombosis. The initial treatment for subacute MVT is mainly conservative and includes anticoagulation, bowel rest, intravenous fluid hydration, and bowel decompression
Conclusions: The presentation of MVT is non-specific and requires a high index of suspicion. In retrospect, had the diagnosis of SMV thrombosis been made earlier from the outside imaging, perhaps this patient could have been initiated on anticoagulation. This would have likely prevented all her complications. This case emphasizes the need to consider mesenteric venous thrombosis in the differential diagnosis of atypical cases of small bowel obstruction.