Background: Since being introduced in the 1950s, midlines have since gained attention as an intravascular access option—particularly in patients requiring intravenous (IV) therapy for extended time periods. They provide an alternative to frequent venipuncture from peipheral intravenous catheters (PIV) and may reduce cost and increase patient satisfaction.
The CDC and MAGIC guidelines currently recommend the use of midlines for patients expecting to need IV therapy for more than 6 days. With the burden of central line associated blood stream infections (CLABSI), midline usage is increasing. Limited data from observational studies suggest an overall positive safety profile with respect to major complications, namely venous thrombosis and line-related infections. In this retrospective study we aimed to quantify the rate of such serious complications associated with the use of midlines.
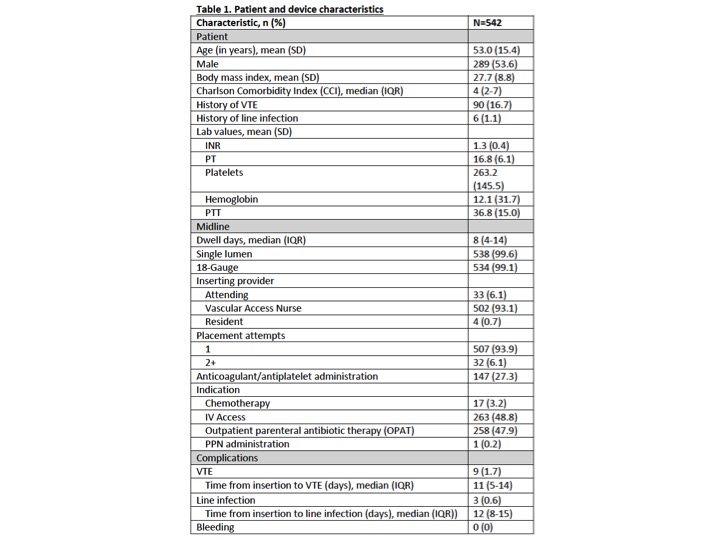
Methods: We retrospectively gathered all midline requests to our vascular access team (VAT) from January 2016 to June 2017 totaling 585 requests. Of these, 539 midlines were placed. The remainder of requests were removed due 1)duplicate request 2)patient refusal 3)vascular access deemed inappropriate or 4)PIV or PICC placed instead. All lines were placed under ultrasound guidance.
Our primary analysis sought to determine the incidence of venous thrombosis and line-related infections in this cohort. We also accounted for patient demographics and clinical conditions as associated factors. The results are presented here.
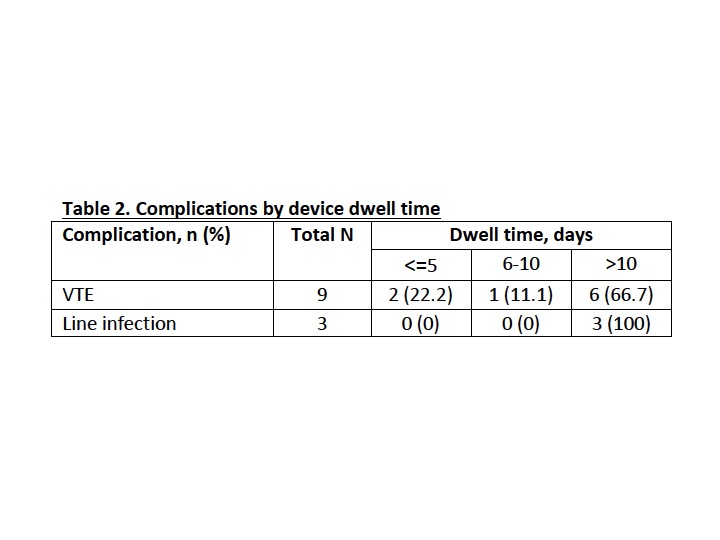
Results: The rate of infectious complications in our study population was less than one percent (n=3; 0.6%), in concordance with the current literature. Infection rates increased with dwell time, with all catheter-related infections occurring after at least 10 days of catheter dwell time. Charlson comorbidity index was calculated for our patients, with a median value of 4. With the overall rate of midline infection still less than one percent there is suggestion that there is safety of the procedure even in patients with higher comorbidity index.
A total of 9 venous thromboses were documented (1.7%). The rate of thrombosis increased with dwell time, with 67% of thrombotic events occuring after 11 days of dwell time, suggesting that the longer the dwell time, the more likely it is for a VTE event to occur. These rates are also similar to that found in existing literature.
Thrombotic and infectious rates are on par with PICC lines, suggesting the use of midlines does not sacrifice safety in appropriately selected clinical situations.
There are some limitations in our study that may provide opportunities for future research. We focused on life-threatening complications and did not address all minor events. This is particularly relevant in the setting of prior studies reporting a higher rate of non-severe complications such as pain, non-patency, leakage and swelling in midlines when compared to PICC. Superficial phlebitis has been reported up to 11% in various midline studies. Our study was also of retrospective nature and prospective validation of findings is necessary.
Conclusions: Midline catheter utilization has increased significantly as an alternative to PICC over the past few decades. The data in our study demonstrate that, based upon low major complications rates, midline catheters are a safe alternative. In patients requiring prolonged intravenous therapy, midline usage can decrease cost, increased patient satisfaction and reduce rates of adverse outcomes, particularly infection and venous thrombosis.