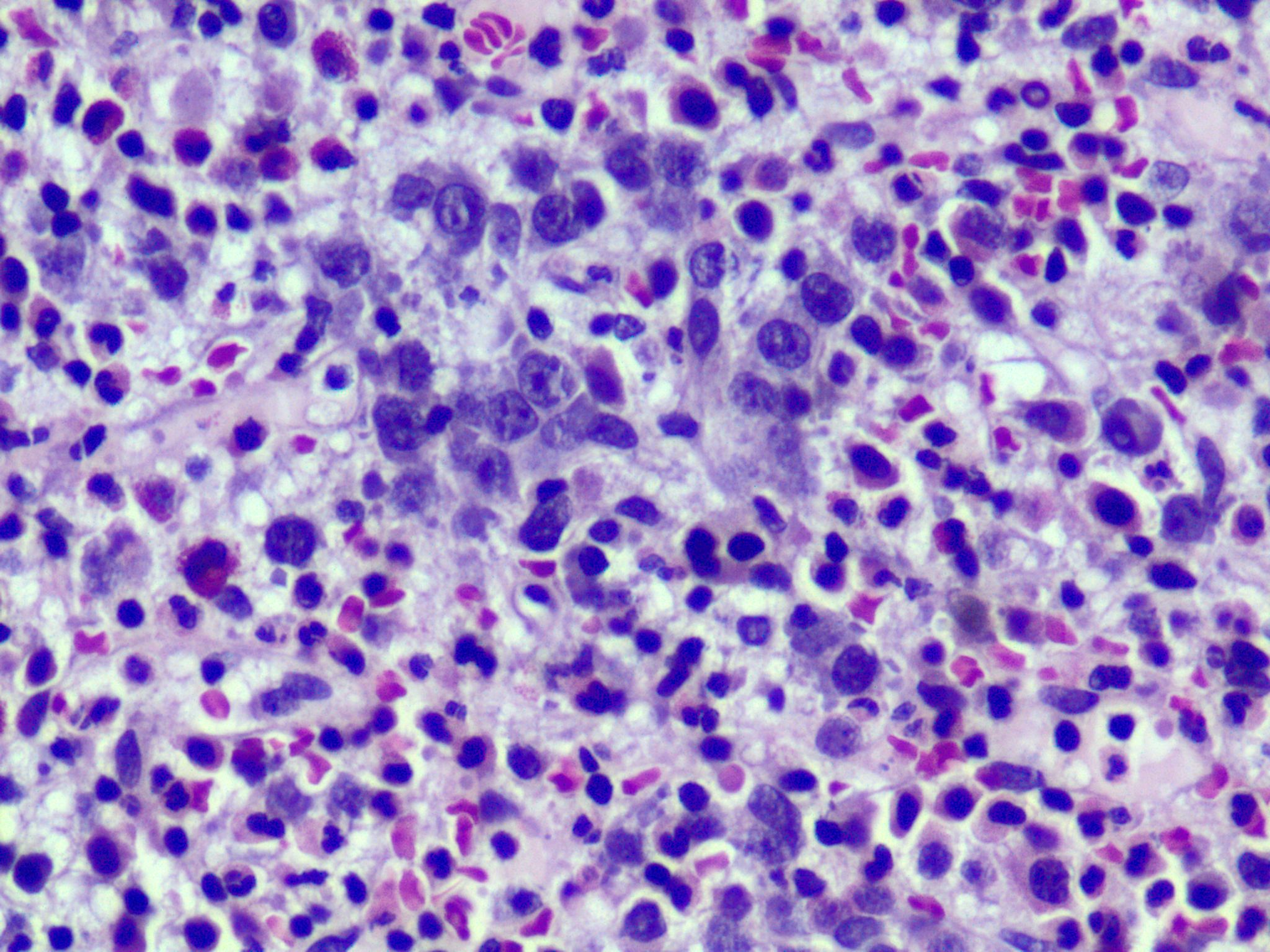
Case Presentation: A 70-year-old male who presented to us with worsening dyspnea on exertion and non-productive cough. Review of systems was negative. Vitals were unremarkable; physical examination was significant for bilateral basilar rales which were corroborated by his chest x-ray that revealed bilateral pleural effusions. Laboratory findings were notable for normocytic anemia and elevated liver function tests which prompted an ultrasound of his abdomen that demonstrated hepatosplenomegaly. While undergoing workup for those mentioned above, his hemoglobin dropped to 6.6 mg/dl from a baseline of 10.6 mg/dl at admission, thus necessitating blood transfusion. Three days later he also experienced an asymptomatic drop in platelets from 181,000 to 36,000 microliter of blood. Additional workup revealed Lactate Dehydrogenase (LDH) of 397, haptoglobin < 15 suggestive of intravascular hemolysis. There was evidence of past (positive serum IgG) but not a current infection (negative IgM) with Cytomegalovirus (CMV), Parvovirus B 19, Mycoplasma, Epstein–Barr virus (EBV), Varicella zoster virus (VCV). Rheumatological work up was negative. Direct Coombs test was positive, and antibody ID was positive for IgG and C3 suggestive of mixed autoimmune hemolytic anemia (AIHA). Bone marrow biopsy revealed a picture concerning for refractory anemia with excess blasts (RAEB)-1. However, flow cytometry was negative. After having ruled out other etiologies for autoimmune hemolytic anemia (AIHA) including non-CMV infections, rheumatological causes, his diagnosis was consistent with CMV related mixed AIHA. The patient received intravenous high dose steroids and was later transitioned to oral steroids at the time of discharge. His hemoglobin and platelets improved remarkably with treatment.
Discussion: Rafailidis et al. (3) performed a systematic review of 290 immunocompetent patients with severe CMV infection, 25 patients were found to have various hematological manifestations among them only five were found have hemolytic anemia, so AIHA is a rare event. AIHA is classified according to Coombs test (Direct Antiglobulin Test (DAT); contains anti-C3 and anti-IgG and thermal characteristics of autoantibody into Warm AIHA (70%), Cold (20%) and Mixed type (0-7%). CMV is known to cause cold AIHA and hasnt been known to cause mixed AIHA. Previously there has only been one case of CMV related mixed AIHA and another of warm AIHA reported in the literature. This is the first report of a mixed AIHA along with thrombocytopenia occurring secondary to CMV. Given it’s rarity, there are no established guidelines to drive management. Supportive care is recommended in mild cases, however, in severe infection steroids, antiviral agents and anti-globulins may be considered on a case by case basis.
Conclusions: Cytomegalovirus can also cause mixed AIHA, not just cold AIHA as previously beleived. Mixed AIHA caused by CMV or other infections responds well to steroids. Low reticulocyte index can be present with severe CMV induced AIHA even though we expect otherwise in patients with hemolytic anemia. Bone marrow findings can mimic refractory anemia with excess blasts (RAEB-1) in patients with autoimmune hemolytic anemia (AIHA) caused by cytomegalovirus (CMV).