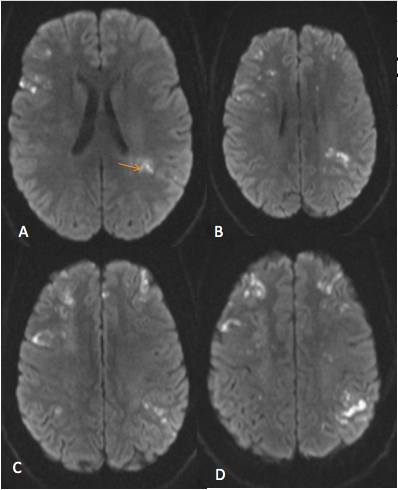
Case Presentation: A 29-year-old African American female, who has a history of preeclampsia and recent stroke, presented with confusion, unusual behavior pattern, headache, involuntary movements and forgetfulness for 3 days. She reported difficulty performing easy tasks such as putting a bottle together, changing her baby and progressive cognitive decline. She denied having weakness, numbness, seizures, fever or chills. She had a strong family history of strokes affecting multiple members at a young age. The patient was awake, alert, oriented with no focal neurologic deficits. Her last stroke had affected her left side but she had no residual weakness. However, she did report urinary incontinence since then. At that time, she was found to have acute bilateral cerebral infarcts with questionable stenosis of bilateral middle cerebral arteries (MCA) and distal right vertebral artery. On this admission, she had further progression of intracranial stenosis and ischemia on imaging. Diagnostic cerebral angiogram showed progressive arteriopathy in both internal carotid arteries (ICA) terminus, and proximal portions of MCA and anterior cerebral arteries (ACA). Series of diagnostic test ruled out infectious causes, rheumatologic disease including primary CNS vasculitis and hypercoagulability disorders. In following with diagnostic criteria we diagnosed our patient with Moyamoya Disease (MMD). We discharged patient with anti-hypertensive medications, high dose statin and dual antiplatelet therapy.
Discussion: Moyamoya disease (MMD) is a chronic cerebrovascular occlusive disease that is characterized by progressive bilateral stenosis of the terminal portion of the internal carotid artery and its main branches (1). Shimizu and Takeuchi first time described it in 1957 in Japan (2). MMD remains rare, especially in African Americans, but is increasing in incidence worldwide (3,4). MMD is an important diagnosis to consider in children, young adults, and individuals who have a significant family history of stroke. Cerebrovascular events are the primary presenting symptoms and are related to both the stenosis and occlusion of the ICAs and its main branches. Detection of bilateral stenosis by cerebral angiography is considered the gold standard, but CTA is also an acceptable method of diagnosis. Although etiology and pathogenesis of MMD remain unclear, genetic factors and inflammation are the most representative two mechanisms. Current literature supports the idea that the complex and multifactorial pathogenesis of MMD cannot be explained by one single mechanism (5). In this report we present a case of a young female who manifested progressive MMD a few months after childbirth.
Conclusions: Careful, long-term neurologic and radiologic follow-up is essential in adult patients with MMD to prevent additional stroke events and improve outcomes. We highly suggest considering MMD as a differential in western countries especially in young patients who presented with progressive cerebrovascular events.