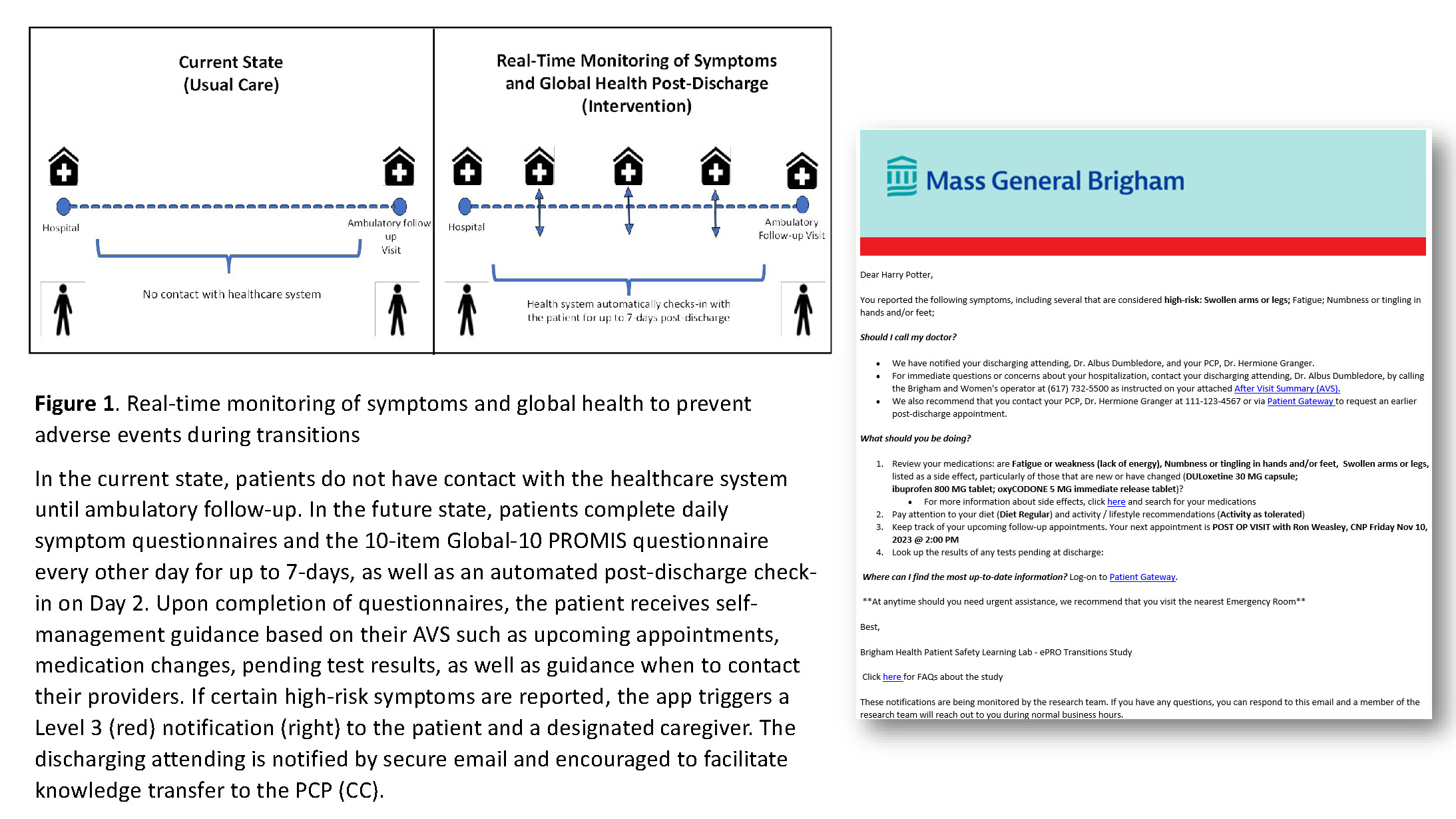
Background: Adverse events (AEs) occur in 19-28% of patients after discharge and can lead to unanticipated events, including emergency room visits and readmissions.(1,2) While early indicators include new and worsening symptoms (NWS), monitoring of patient-reported NWS is lacking. The 21st Century Cures Act mandates adoption of application programming interfaces (APIs), offering the potential to engage patients via interoperable apps during their transition home (Figure 1) through automated check-ins as well as individualized risk assessments derived from questionnaire and electronic health record (EHR) data typically included in after-visit summaries (AVS). Escalation of high-risk states may lead to earlier detection of these AEs.
Purpose: As part of a 5-year AHRQ project (R01-HS028662), we report our experience developing and piloting MyPostDischargePal, an EHR-interoperable app to support patients with multiple chronic conditions in AE surveillance during transitions.
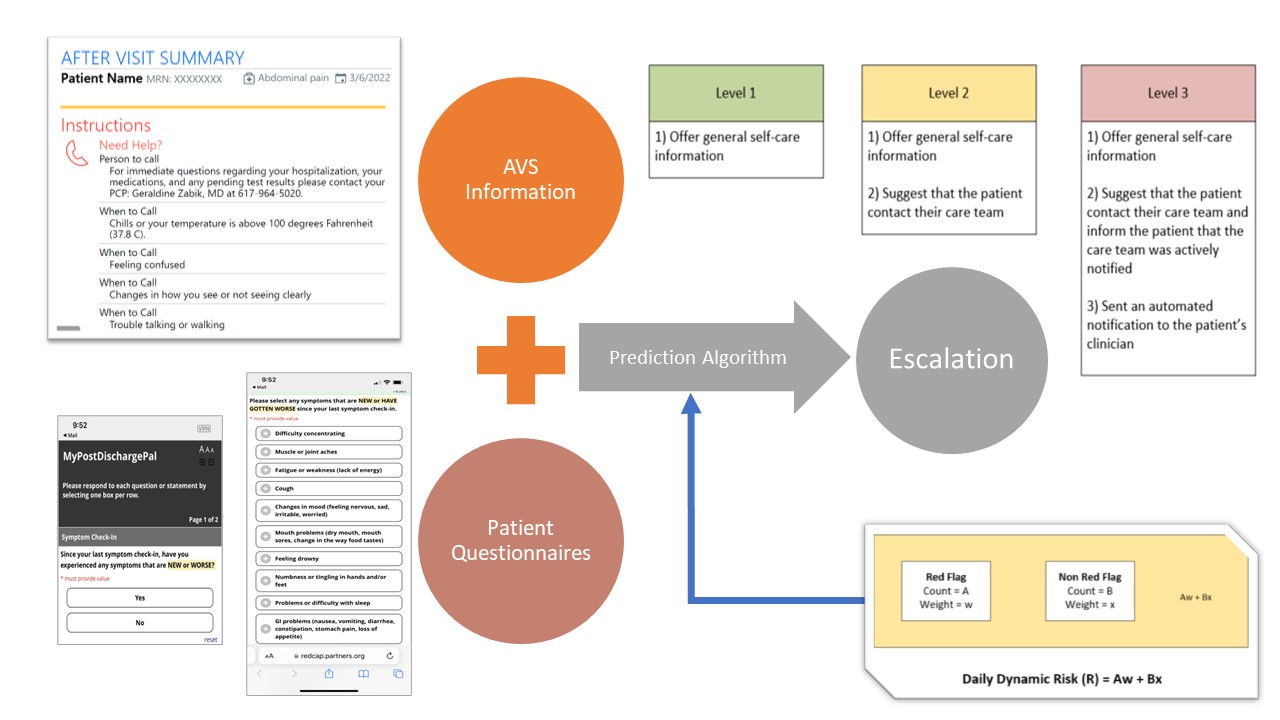
Description: We gathered user requirements from 13 patients and 12 clinicians (5 hospitalists, 5 advanced practice providers, 2 primary care providers (PCP)) to develop a functional prototype of the MyPostDischargePal app in REDCap (Figure 2). We collected feedback and iteratively refined the app’s functionality (self-management advice, escalation logic, user-interface) during 12 rounds of mock-testing with the research team, clinician-working group members, patient advisors, and external stakeholders. Patients complete daily symptom and global-10 patient-reported outcome (PRO) questionnaires for 7-days post-discharge. The app triggers 3 levels of escalation (green, yellow, red) based on an escalation algorithm that incorporates patient-reported NWS from questionnaires.(3) The app provides pertinent AVS information (upcoming appointments, medication changes, pending test results) retrieved from the EHR via APIs and links to validated education resources (MedlinePlus). Of 15 patients enrolled to date, 12 (80%) completed at least one questionnaire after discharge. Of these 12, 9 (75%) completed >70% of questionnaires. Mean (SD) mental and physical health PRO scores during the 7-days were 42.3 (1.97) and 40.8 (2.56), respectively. Of the 3 patients who reported high-risk NWS triggering a Level 3 (red) escalation (Figure 1), 2 had an emergency room visit within 7-days. Preliminary feedback from 6 patient interviews suggest that the questionnaires and escalation notifications were clear, easy to follow, well-timed, and provided helpful links to the AVS. Comments suggested that app users felt supported: “You go from 24-hour care to home which can be jarring, so it was nice to have the [app] surveys” – patient 1; “[I] felt-taken care of” – patient 2. Initial clinician feedback underscores the importance of clarifying responsibility between attending and PCP.
Conclusions: Remote monitoring of NWS and global health, and escalation of potential AEs via an interoperable app is acceptable and feasible for general medicine patients transitioning home. We observed high adherence and targeted escalation of at-risk patients who experienced a potential AE soon after discharge. Our next steps are to incorporate additional EHR data and PRO score trends to improve AE risk prediction, leverage generative AI to facilitate PRO score interpretation, clarify clinician responsibility for post-discharge escalation events, and conduct randomized controlled trial to evaluate impact of this intervention on post-discharge outcomes.