Background: Inpatient phlebotomy-associated-anemia (PAA) has garnered significant attention in recent years, with numerous studies delving into this common and preventable condition’s implications for patient outcomes. During hospitalization, it is estimated that about 18% of patients develop anemia associated with phlebotomy. We evaluated the prevalence and impact of PAA at Grady Memorial, a public safety-net hospital. Once the prevalence was identified, we performed targeted education to providers to use the available blood-conservation laboratory (lab) panel that requires only 3 mL of blood as compared to the 10 mL of blood needed for traditional lab testing.
Methods: A retrospective chart review was conducted on 200 patients admitted between May 2022 and March 2023. Patients with medical conditions that might have contributed to anemia, either upon admission or during their hospital stay (active gastrointestinal bleeding, hemolysis, hematuria, hemoptysis, hemorrhagic stroke, hemothorax, bleeding cutaneous ulcers, hemarthrosis, retroperitoneal bleeding, or hematological malignancies), those on therapy that could affect hemoglobin/hematocrit levels (iron, chemotherapy, or erythropoietin), those on dialysis, and those who received a red blood cell transfusion were all excluded from this study. Other excluding factors included patients with BUN/Cr ratio greater than 25, presentation suggesting possible gastrointestinal bleeding. After applying the exclusion criteria only 47 out of 200 patients were deemed eligible for the study. The charts of the 47 patients were reviewed from Day 1 to Day 5 of inpatient hospitalizations to assess any drop in hemoglobin levels. For this study, a significant decrease in hemoglobin is defined as a patient with a hemoglobin decrease of more than 0.7 g/dL.
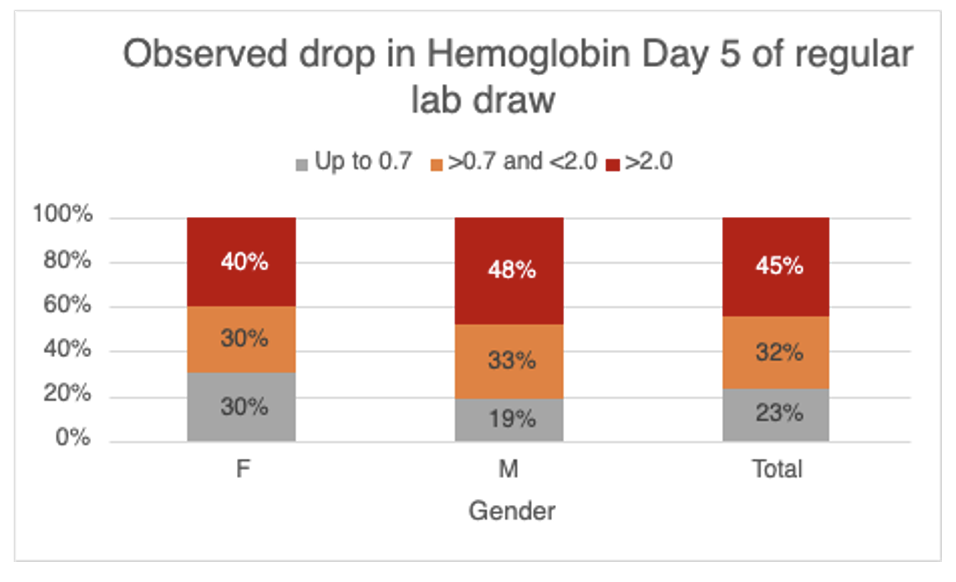
Results: Out of 47 patients, 23.5% had a diagnosis of anemia and 76.5% did not have a diagnosis of anemia on day 1. On day 5, 77% of 47 patients experienced significant drops in hemoglobin levels, out of the 77%, 45% experienced a drop of more than 2 g/dL and 32% a drop of 0.8-2 g/dL. Among the 76.5% of 47 patients with no anemia on admission, 50% were diagnosed with anemia by day 5. In efforts to decrease PAA, targeted education (via epic-chat, e-mail and huddles) were conducted to remind the providers about the conservation-lab panel for common lab studies. Following 17 weeks of these efforts, we saw an initial rise in the utilization of blood-conservation labs in the first 4 weeks, but this was followed by a decline in use.
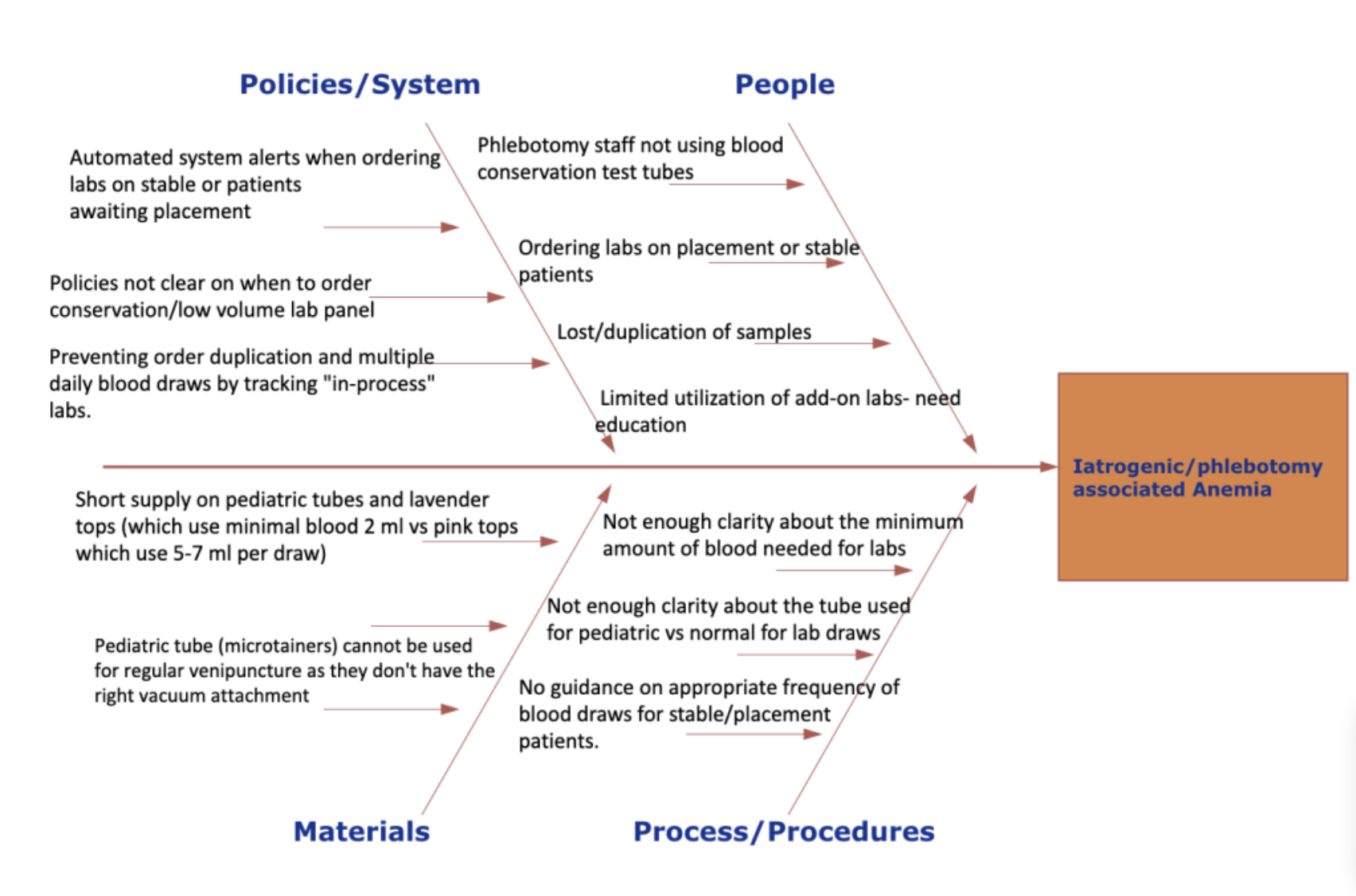
Conclusions: Blood loss from PAA as we surmise is underreported and overlooked. PAA has previously been reported to be associated with poor patient outcomes, increased length of stay and healthcare cost burden. Our study highlights that PAA is prevalent at Grady Hospital. Initial attempts at targeted education to encourage the use of blood-conservation lab panels were initially successful but this was followed by a decline likely due to its non-intuitive nature and provider forgetfulness. In the future, we aim to not only provide providers with a report-out of their individual lab utilization but also to provide focused education efforts on common inpatient diagnoses that do not need more frequent laboratory monitoring. Lastly, we seek to harness technology through electronic medical records to preferentially select blood-conservation lab panels for patients with documented anemia. With these targeted interventions, we hope to decrease the incidence of PAA while still offering high quality patient care.