Background: Endovascular cardiac valve replacement continues to increase in popularity as it becomes more of a standard of care for valve replacements. As the number of ECVR grows each year, complications associated with these procedures may elevate the cost and limit the viability of these procedures in healthcare systems. Hospitalists need to be aware of these implications when it comes to assuring cost-effective care nationwide. This study seeks to evaluate the costs associated with ECVR and their complications, as well as helping to predict negative effects in our healthcare system.
Methods: Our study included population derived from the United States National Inpatient Sample (NIS) database. We included patients who underwent ECVR during a 1-year period, using the Medicare-Severity Diagnosis Related Groups (MS-DRG) code 266 (endovascular cardiac valve replacement with complications or comorbidities) and 267 (endovascular cardiac valve replacement). We analyzed patient demographics, hospital costs and charges, length of stay and total treatment aggregate charges and costs. Statistical analyses was performed using the Z-test, in order to determine the association between nominal variables such as complicated and non-complicated procedures, income status and patient age group, as well as continuous variables including hospital length of stay, charges and costs. We determined statistical significance as a p value ≤0.01 in order to reach a greater power.
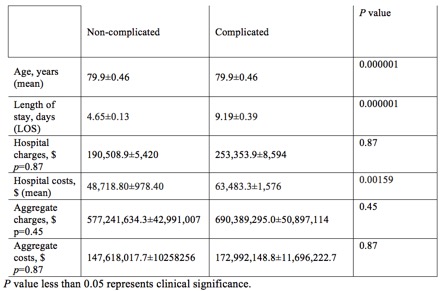
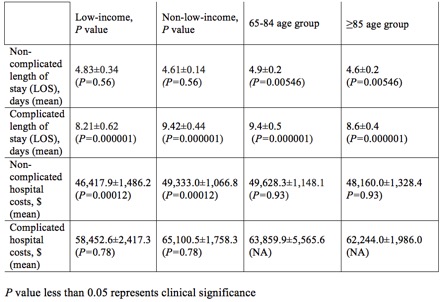
Results: Of 5755 patients, 2724 (47.4%) were found to have associated procedural complications. We found that those with complications were slightly older than those without (mean age of 79.9±0.46 vs. 79.8±0.58, p value=0.000001). The presence of complications was also associated with an increased length of hospital stay (9.19±0.39 days vs. 4.65±0.13 days, p value=0.000001). Hospital costs also appeared to be increased in the group that developed complications compared to the non-complication group ($63,483.3±1,576 USD vs. $48,718.80±978.40, p value=0.00159). Differences in hospital charges, aggregate charges or aggregate costs were not statistically significant. When evaluating the complication group by economic sub-groups, we found that the low-income population had a shorter length of stay compared to the higher-income population (8.211±0.62 days vs 9.43±0.423 days, p value=0.000001). In the non-complication group, we did not find any significant length of stay difference in low-income vs higher-income sub-groups (4.83±0.34 days vs 4.61±0.14 days, p value=0.555). Low-income patients were also associated with lower hospital costs per admission compared to higher-income patients in the non-complication group ($46,417±1,486 USD vs. $49,332±1,066 USD, p value=0.00012). Finally, length of stay appeared to be longer in younger patients than older among patients with procedural complications (9.38±0.52 days in 65-84 year olds vs. 8.59±0.44 days in those ages ≥85, p value=0.000001).
Conclusions: This study provides perspective on the nationwide expenses that are incurred when patients undergoing ECVR develop complications. Higher-income and younger populations appeared to have longer lengths of stay which may translate to increased costs in the healthcare system. Further studies with the overall intent to target the prevention of complications of these procedures are needed to better mitigate potential economic burden on our healthcare systems.