Background: General medicine consultation (GMC) requires familiarity with consultative medicine and effective collaboration, as well as understanding distinctions between consultation and co-management.1-6 Although GMC is a requirement of internal medicine training, little guidance exists in developing curricula, and co-management may be neglected.2 A GMC curriculum exists within the Section of Hospital Medicine at University of Chicago, but it is broad in scope, not data driven, and has not been updated in nearly a decade. Additionally, during this period new co-management models with surgical services were developed. Recent work indicates possible overuse in co-management-based consultation practices.6 Changing needs in consultation and co-management require increased attention to the landscape of GMC and how to tailor curricula better to the needs of trainees and collaborating specialties.
Purpose: We performed a chart review-based needs assessment to describe problems requested by consulting services with the goal of developing an updated inpatient GMC curriculum. We additionally compared problems addressed per consult to problems requested to better understand scope of consultation amongst consultative and co-management models.
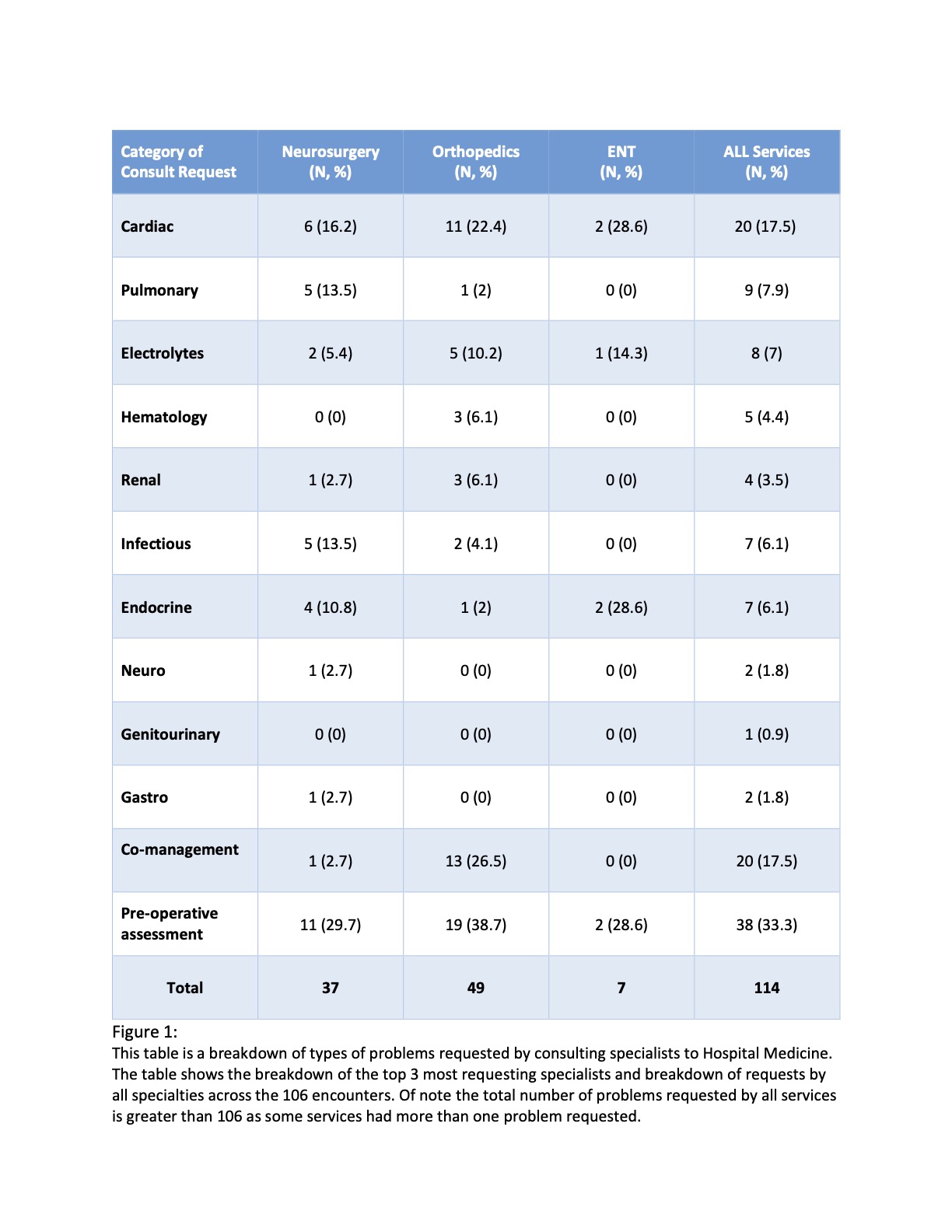
Description: A retrospective study from a time-limited sample from July 2019-June 2020 of approximately 500 charts in our EMR, 106 charts were randomly selected for a preliminary analysis. Expedited IRB approval was obtained. Chart information abstracted by 4 raters included GMC type (consultative vs co-management), requesting service, consult problems requested, and problems addressed in consult. Consensus on abstraction was achieved via discussion. Descriptive statistics were performed. Surgical specialists (93%) comprising orthopedics (41%), neurosurgery (25%), and ENT (6%) most commonly requested GMC (Figure 1). Overall, the most common problem requested for GMC was pre-op evaluation (33%); co-management was requested in 17%. Figure 1 displays most common reasons for GMC by specialty. Consult problem varied by specialty; neurosurgery most commonly requested pre-op evaluation (30%), followed by cardiac (16%, top problem blood pressure management) and pulmonary problems (14%, top problem hypoxia). Orthopedics most commonly requested pre-op (39%), followed by cardiac problems (22%, arrythmia and blood pressure top problems). Hospitalists addressed more problems than requested in 38% of GMCs, with mean 4.45 problems addressed in these instances vs. mean 1.07 problems requested.
Conclusions: In our preliminary analysis, orthopedics and neurosurgery requested GMCs most frequently. Most common reasons for GMC showed considerable overlap but varied somewhat by specialty. If trends established in our preliminary findings are consistent with complete analysis, next steps include revamping our educational curriculum with a strong focus on pre-operative evaluation, cardiac issues, and principles in co-management to match our findings. We were surprised by the finding that consultant hospitalists address more medical issues than requested. Over-addressing issues in GMC may be associated with greater morbidity and mortality7, and our findings suggest the need to improve consult specificity and communication. Once completed, our needs assessment will help reshape GMC education for trainees, direct faculty development, and improve partnerships with co-management services.